Ativan (lorazepam), a widely prescribed benzodiazepine, is used to manage anxiety disorders due to its calming effects on the central nervous system. Understanding how long this medication stays in your system is crucial, especially to prevent potentially severe drug interactions. Ativan can be detected in your urine for up to six days, in your blood for up to three days, and in hair follicles for 30 days or longer (Mayo Clinic, 2025). Its presence in the body, combined with other substances, carries risks, including the possibility of fatal respiratory depression. This guide outlines how Ativan is processed, key detection timelines, and vital steps to avoid dangerous medication combinations.
Table of Contents
- Understanding Ativan: Purpose and Effects
- Ativan's Journey: How Long It Stays in Your System
- Factors Influencing Ativan Detection Times
- Proactively Avoiding Severe Drug Interactions with Ativan
- Managing Ativan Use: Precautions and Overdose Risks
- Safe Ativan Discontinuation and Getting Support
1. Understanding Ativan: Purpose and Effects
Ativan, scientifically known as lorazepam, belongs to the benzodiazepine class of drugs, primarily prescribed for its sedative and anxiolytic properties. It effectively treats anxiety disorders by enhancing the effects of gamma-aminobutyric acid (GABA), a natural neurotransmitter in the brain (Harvard, 2024). This enhancement leads to a reduction in brain activity, inducing a calming and relaxing effect on the central nervous system. It's often chosen for its rapid onset of action, providing quick relief for acute anxiety or panic attacks.
The medication can be administered in various forms, including tablets, liquid concentrates, or by injection, each with a distinct timeline for effectiveness. Oral forms typically reach their peak effects within two hours, offering sustained relief. In contrast, an injected dose can begin to take effect within 15 minutes, with its calming properties lasting approximately six to eight hours (FDA, 2025). Despite its rapid action, Ativan has a relatively long half-life, meaning it takes a significant amount of time for its concentration in the body to reduce by half. This characteristic contributes to its lasting presence in the system and is a key factor when considering potential severe drug interactions with other medications that have prolonged effects. Given its potent impact on the CNS, understanding its full duration of action and elimination process is paramount for patient safety.
2. Ativan's Journey: How Long It Stays in Your System
Ativan's journey through the body involves absorption, metabolism, and elimination, impacting how long it remains detectable. The drug is primarily metabolized by the liver, where it is converted into inactive compounds. These metabolites are then largely excreted by the kidneys, predominantly through urine (NIH, 2025). While Ativan is known for its fast-acting nature, its half-life of roughly 12 hours means it takes several half-lives for the drug to be completely cleared from the body. This extended clearance time is crucial for patients and healthcare providers to monitor, especially when considering new medications to avoid severe drug interactions.
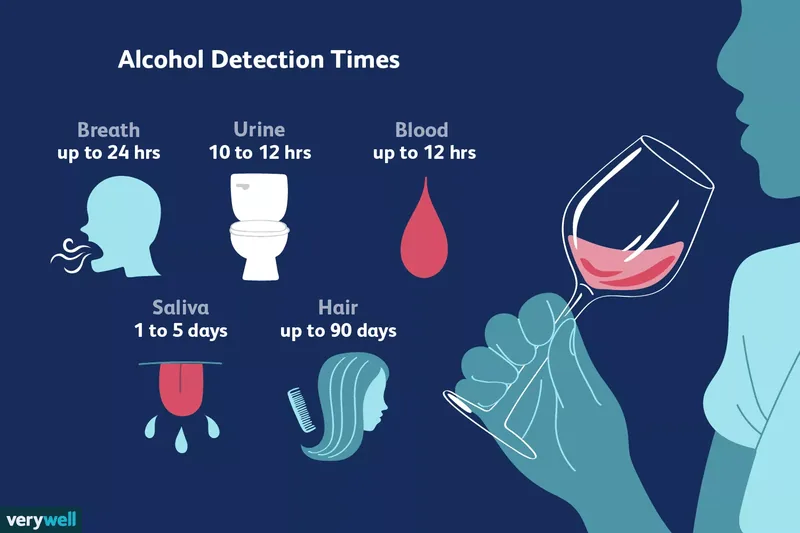
The presence of Ativan can be detected through various drug screening methods, each offering a different window of detection:
- Urine: Ativan metabolites can typically be detected in urine for up to six days after the last dose (Mayo Clinic, 2025). For individuals on higher doses or long-term therapy, this window can extend. Specific tests looking for lorazepam-glucuronide, a primary metabolite with a longer half-life, might detect the drug for up to eight days.
- Blood: Blood tests can identify Ativan as early as six hours post-ingestion and can remain positive for up to three days. Chronic users or those on high doses may show longer detection periods.
- Hair: Hair follicle tests offer the longest detection window, capable of identifying Ativan for up to 30 days or even longer after use. This method captures a historical record of drug exposure, making it useful for long-term monitoring.
- Saliva: Although less commonly used for benzodiazepine screening, older research suggests Ativan can be detected in saliva samples for up to eight hours following administration (Forensic Science International, 2004).
It is important to disclose any Ativan prescriptions to testing laboratories to ensure accurate interpretation of results. False positives can occur with certain antidepressants like Zoloft (sertraline) or antiviral drugs such as efavirenz, highlighting the need for complete medication disclosure (Schwebach & Ball, 2016).
3. Factors Influencing Ativan Detection Times
The duration Ativan remains in a person's system is not uniform; a multitude of factors can significantly influence its metabolism and elimination rates. Understanding these variables is crucial for both personal safety and accurate medical assessments. While general timelines exist, individual physiological differences can lead to quicker or slower clearance of the drug, impacting the risk of severe drug interactions if new medications are introduced.
Key biological factors that affect how long Ativan stays in your body include:
- Age: Older individuals typically metabolize and excrete medications at a slower rate than younger adults. This is attributed to age-related physiological changes such as reduced organ function, decreased blood flow, and slower metabolic processes (NIH, 2025). Consequently, an older patient might experience Ativan's effects for a longer period, increasing their susceptibility to prolonged sedation or interactions.
- Kidney Function: While liver impairment has a minimal impact on Ativan's clearance, compromised kidney function is directly associated with a prolonged drug half-life. Since the kidneys are the primary route for eliminating Ativan's metabolites, impaired renal function means the drug stays in the system longer, raising the potential for accumulation and adverse effects (FDA, 2025).
- Body Composition: Factors like height, weight, and overall body mass can influence drug distribution and metabolism. Generally, individuals with higher body mass might clear the drug more quickly due to greater volume of distribution, though this is not a universal rule and depends on other metabolic factors.
- Genetics: Genetic variations in liver enzymes responsible for drug metabolism can also play a role. Some individuals may be "fast metabolizers" while others are "slow metabolizers," leading to differing drug clearance rates.
Beyond biological predispositions, the specifics of Ativan use itself play a significant role. Higher doses naturally take longer for the body to process and eliminate. Similarly, individuals who have been taking Ativan regularly or for an extended period will have a longer detection window compared to those who use it sporadically or for short durations. The body may adapt to chronic exposure, and accumulation can occur, prolonging its presence. Furthermore, the concurrent use of other substances, whether prescription medications, over-the-counter drugs, or illicit substances, can profoundly impact Ativan's metabolism. For instance, some medications, like the mood stabilizer valproate, can significantly reduce lorazepam clearance, thereby increasing the risk of severe drug interactions (FDA, 2025). Conversely, certain oral contraceptives might accelerate its elimination. Always disclose all medications and supplements to your healthcare provider to mitigate these risks.
4. Proactively Avoiding Severe Drug Interactions with Ativan
Preventing severe drug interactions with Ativan is paramount for patient safety, as certain combinations can lead to life-threatening complications. Ativan is a central nervous system (CNS) depressant, meaning it slows down brain activity. When combined with other substances that also depress the CNS, the effects can be dangerously amplified, leading to profound sedation, respiratory depression, coma, or even death (Harvard, 2024). This section outlines crucial steps and examples to proactively avoid such critical medication risks.
The most critical interaction to avoid is the combination of Ativan with alcohol. Both substances are powerful CNS depressants, and their combined effect is synergistic, not merely additive. Even small amounts of alcohol can significantly increase Ativan's sedative effects, leading to extreme drowsiness, impaired coordination, and a severe reduction in breathing rate (NIH, 2025). This combination is a leading cause of overdose fatalities involving benzodiazepines. Similarly, opiate medications, such as hydrocodone, oxycodone, fentanyl, and morphine, present an equally perilous risk. Opiates are also potent CNS depressants, and when taken with Ativan, they dramatically increase the likelihood of respiratory arrest. Healthcare providers typically issue black box warnings against co-prescribing these drugs unless absolutely necessary and with extreme caution.
To proactively mitigate the risk of severe drug interactions, meticulous communication with your healthcare provider is essential. Always provide a comprehensive list of all medications you are currently taking, including prescription drugs, over-the-counter remedies, herbal supplements, and vitamins. Be explicit about any recreational drug use or alcohol consumption. For example, some antihistamines (like diphenhydramine) or muscle relaxants (like cyclobenzaprine) also have CNS depressant effects and can contribute to dangerous sedation when combined with Ativan. Even seemingly innocuous supplements like St. John's Wort could potentially affect how Ativan is metabolized, although the primary concern lies with other depressants. Your doctor can then assess potential interactions and adjust dosages or recommend alternative treatments to ensure your safety. Never start or stop any medication or supplement without consulting your physician, especially when taking Ativan, as this can inadvertently lead to dangerous drug combinations or withdrawal symptoms. Being informed and proactive is your best defense against serious adverse reactions.
5. Managing Ativan Use: Precautions and Overdose Risks
Managing Ativan use requires strict adherence to prescribed guidelines and a thorough understanding of its associated risks, particularly concerning overdose and severe drug interactions. Ativan is classified as a Schedule IV drug, indicating a lower potential for misuse compared to Schedule II or III substances; however, it can still be habit-forming (DEA, 2024). For this reason, it is typically prescribed for short-term use to minimize the risk of developing tolerance and dependence. Long-term use can lead to physical dependence, where the body adapts to the drug's presence, requiring higher doses to achieve the same therapeutic effect and leading to withdrawal symptoms if stopped abruptly.
The risk of overdose is a serious concern, most frequently observed when Ativan is combined with other CNS depressants, notably alcohol or opioid medications. This combination creates a synergistic effect, profoundly suppressing the central nervous system and leading to life-threatening conditions. Signs of an Ativan overdose include confusion, severe drowsiness, poor coordination, slowed reflexes, slurred speech, and potentially coma or death (NAMI, 2025). It is crucial for family members or caregivers to be aware of these symptoms and to seek immediate emergency medical help by calling 911 if an overdose is suspected. This proactive awareness is vital in preventing tragic outcomes from severe drug interactions.
Beyond interactions with alcohol and opioids, several other precautions are critical for safe Ativan use:
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss this with your doctor. Ativan can pass into breast milk and may affect the baby (Anderson, 2022). Its use during pregnancy should be carefully weighed against potential risks to the fetus.
- Mental Health Conditions: Individuals with depression or suicidal thoughts should generally avoid Ativan, as it can sometimes exacerbate these conditions.
- Elderly Patients: Older adults may be more susceptible to Ativan's effects, such as drowsiness and impaired coordination, increasing their risk of falls. Dosage adjustments are often necessary for this population.
- Smoking: Tobacco use can reduce the effectiveness of Ativan, potentially requiring higher doses and increasing overall exposure.
- Other Medications: Always inform your doctor about all prescription and over-the-counter medications, supplements, and herbal products you are taking. Many drugs, even those not directly affecting the CNS, can alter Ativan's metabolism or clearance, leading to unexpected and potentially severe drug interactions. For instance, certain antibiotics or antifungals could interfere with the liver enzymes responsible for breaking down Ativan.
Adhering to these precautions and maintaining open communication with your healthcare provider are fundamental steps in safely managing Ativan therapy and minimizing the risks of adverse events.
6. Safe Ativan Discontinuation and Getting Support
Discontinuing Ativan, especially after prolonged use, requires careful planning and medical supervision to prevent potentially severe withdrawal symptoms. Physical dependence can develop even when the drug is taken exactly as prescribed, making abrupt cessation dangerous. Quitting Ativan suddenly can trigger a range of withdrawal effects, including heightened anxiety, insomnia, irritability, tremors, and in severe cases, seizures, which can be life-threatening (Brett & Murnion, 2015). Therefore, a supervised tapering schedule is the standard and safest approach.
Your physician will guide you through a gradual reduction of your Ativan dosage over a period, allowing your body to slowly adjust to decreasing levels of the medication. This controlled reduction minimizes the intensity of withdrawal symptoms and helps prevent serious complications. While there are no specific medications approved solely for treating Ativan dependence, the tapering process itself is a medical intervention designed to manage withdrawal effectively. Regular check-ins with your doctor during this period are essential to monitor your progress and adjust the tapering schedule as needed. This process also helps identify any resurgence of underlying anxiety or other conditions that Ativan was initially prescribed to treat, allowing for alternative management strategies.
Beyond the physical aspects of discontinuation, psychological support is often beneficial. Your healthcare provider may recommend psychotherapy, such as cognitive-behavioral therapy (CBT) or dialectical behavioral therapy (DBT), which can provide coping mechanisms and strategies for managing anxiety without medication (Carroll & Kiluk, 2017). These therapies help individuals address the root causes of their anxiety and develop healthier thought patterns and behaviors. For those struggling with substance use or addiction related to Ativan, seeking specialized addiction recovery services is crucial. Mental health professionals specializing in addiction can offer tailored support, including individual counseling, group therapy, and relapse prevention strategies. If you or a loved one are facing challenges with Ativan use or dependence, reaching out for professional help is a vital step toward recovery. Your physician can provide referrals to psychiatrists, therapists, or addiction specialists who can offer comprehensive care and guidance through this process, ensuring a safe and supported path to discontinuation and sustained well-being, free from the risks of dependence and severe drug interactions.