Our bodies are intricate systems, constantly communicating internally to keep us moving, thinking, and feeling. At the heart of this communication lies a vital chemical messenger: acetylcholine. This powerful neurotransmitter plays a fundamental role in how acetylcholine functions in your body, orchestrating everything from the blink of an eye to the formation of new memories. Understanding its mechanisms is key to appreciating overall health and cognitive performance.
Acetylcholine (ACh) is a neurotransmitter that transmits signals between nerve cells, enabling muscle contraction, regulating vital organ functions, and supporting critical brain processes like learning and memory. Its widespread influence means that optimal acetylcholine functions in the body are essential for daily physical and mental well-being. This guide will explore the profound impact of this chemical messenger.
Prerequisites for Understanding Acetylcholine
To fully grasp how acetylcholine functions in the body, it’s helpful to have a basic understanding of the nervous system. This includes knowing the difference between the central nervous system (CNS – brain and spinal cord) and the peripheral nervous system (PNS – nerves outside the CNS). Neurotransmitters are chemical messengers that carry signals across synapses, which are the junctions between nerve cells.
Additionally, familiarity with the concept of nutrients impacting brain health is beneficial. Specifically, recognizing choline as an essential nutrient for acetylcholine synthesis provides crucial context. This foundational knowledge will make the intricate roles of acetylcholine clearer and more accessible.
1. Understanding Acetylcholine: The Master Neurotransmitter
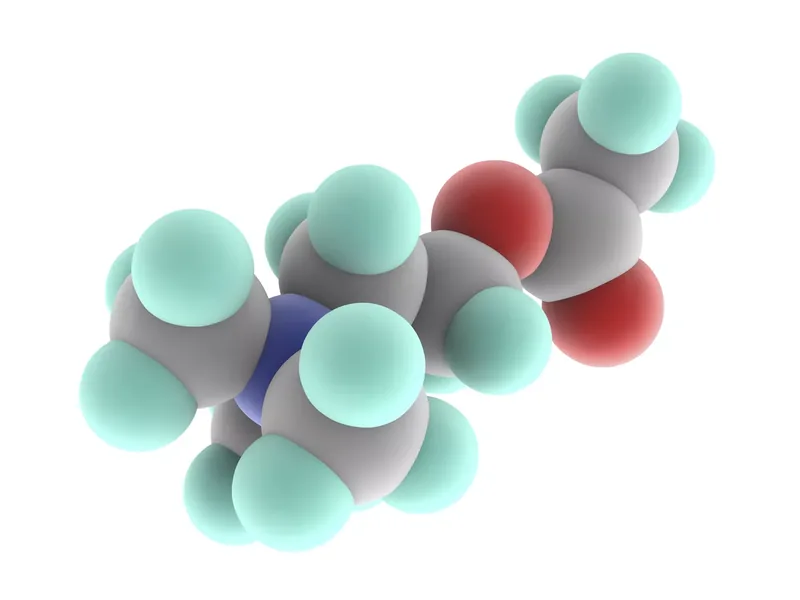
Acetylcholine (ACh) stands as a foundational neurotransmitter, critical for the vast network of communication within our nervous system. It’s a chemical compound derived from acetic acid and choline, specifically designed to transmit signals efficiently across synapses. Discovered over a century ago, its profound importance continues to be a subject of intense scientific study, with current research (2025) consistently revealing new facets of its role (leading research, Harvard, 2024).
What makes acetylcholine so pivotal is its dual role: it operates in both the central nervous system and the peripheral nervous system. This widespread presence means that its influence touches nearly every aspect of our physical and mental existence. From the smallest involuntary reflex to complex thought processes, understanding how acetylcholine functions in the body is like uncovering a key controller for our entire biological machinery. This master neurotransmitter ensures that electrical signals are converted into chemical messages, which then trigger new electrical signals in receiving cells.
In the CNS, acetylcholine acts as a neuromodulator, fine-tuning brain activity related to attention, learning, and memory. Meanwhile, in the PNS, it serves as the primary neurotransmitter for the somatic nervous system, directly activating muscles for voluntary movement. It also plays a significant role in the autonomic nervous system, influencing heart rate, digestion, and other involuntary bodily processes. This comprehensive involvement underscores why disruptions to acetylcholine pathways can have such far-reaching consequences for health and well-being.
The term “master neurotransmitter” isn’t an exaggeration, given its extensive reach and the diversity of its responsibilities. Whether it’s initiating a muscle contraction or helping you recall a distant memory, acetylcholine is continuously at work. Its precise regulation is vital for maintaining physiological balance and cognitive sharpness throughout life, making it a cornerstone of neurological function.
2. Core Functions of Acetylcholine in the Body
The primary function of acetylcholine in the body is to facilitate communication that leads to action, particularly in muscle movement and autonomic regulation. It is found universally in motor neurons, where its release at neuromuscular junctions directly stimulates muscles to contract. This critical function underpins all physical activity, from the powerful pump of your heart to the delicate movements of your fingers.
Consider the intricate process of playing a musical instrument, like the piano. Each note requires precise, coordinated muscle contractions in your hands and fingers. This entire complex sequence is initiated and sustained by acetylcholine. A signal from the brain travels down nerve fibers, releasing ACh at the neuromuscular junction, which then triggers the specific muscle fibers to contract, allowing you to hit the right key at the right time. Without optimal acetylcholine functions in the body, such fine motor control would be impossible.
In the peripheral nervous system (PNS), acetylcholine’s influence extends to both voluntary and involuntary actions. Within the somatic nervous system, it acts as an excitatory neurotransmitter, directly causing skeletal muscles to contract. This ensures that when your brain decides to move your arm, the message is effectively delivered and executed by the target muscles.
Furthermore, within the autonomic nervous system, acetylcholine plays a crucial role in regulating involuntary body functions. It is a key player in the parasympathetic nervous system, responsible for “rest and digest” responses. For instance, acetylcholine slows the heart rate, increases digestive secretions, and promotes the contraction of smooth muscles in organs like the bladder. A new example is its role in bladder control: the sensation of needing to urinate and the subsequent contraction of bladder muscles for emptying are largely mediated by acetylcholine, ensuring proper waste elimination. This shows the profound impact of how acetylcholine functions in the body on everyday physiological processes.
3. Acetylcholine’s Impact on Cognition and Behavior
Beyond its role in physical movement, acetylcholine is a powerhouse within the central nervous system, profoundly influencing our cognitive abilities and behaviors. It acts as both a neurotransmitter and a neuromodulator in various brain regions, shaping how we learn, remember, and perceive the world. Optimal acetylcholine functions in the body are paramount for maintaining sharp mental acuity.
One of its most significant contributions is to learning and memory. Acetylcholine is crucial for neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections. This process is fundamental to acquiring new knowledge and skills, making acetylcholine indispensable for academic learning and professional development. When you are trying to master a new language or understand complex concepts, acetylcholine is actively working to facilitate the necessary changes in your brain.
Moreover, acetylcholine plays a vital role in attention and arousal. It helps us focus on specific tasks by triggering a process known as sensory gating. This mechanism effectively reduces or blocks out background noise and irrelevant stimuli, allowing us to concentrate on what’s important. For example, during a busy workday in an open-plan office, your ability to maintain focus on a complex report despite surrounding conversations and distractions is significantly aided by acetylcholine. This filtering capacity is a prime example of how acetylcholine functions in the body to enhance behavioral efficiency.
The neurotransmitter is also deeply involved in promoting REM (Rapid Eye Movement) sleep, the stage of sleep associated with vivid dreaming and memory consolidation. Disruptions in acetylcholine levels can therefore impact sleep quality and, consequently, cognitive performance. Its influence on motivation means it can also affect our drive to engage with tasks and pursue goals. The intricate interplay of acetylcholine with other brain chemicals ensures a balanced and responsive cognitive landscape.
4. The Choline Connection: Fueling Acetylcholine Production
The production of acetylcholine is a finely tuned biological process that relies heavily on a crucial precursor: choline. Choline is an essential nutrient, meaning our bodies cannot produce enough of it on their own to meet demand, necessitating its acquisition through diet. Without adequate choline, the synthesis of acetylcholine is compromised, directly impacting how acetylcholine functions in the body.
Acetylcholine production primarily occurs in the nerve terminals of cholinergic neurons. Here, an enzyme called choline acetyltransferase facilitates the chemical reaction that combines choline with acetyl-CoA to form acetylcholine. This biochemical pathway is continuous, ensuring a steady supply of the neurotransmitter for ongoing nerve signaling. Therefore, the availability of dietary choline is a direct determinant of the brain’s capacity to produce this vital chemical messenger.
A lack of sufficient choline in the diet can lead to a range of negative health consequences. For instance, it can impair the liver’s ability to process fats, increasing the risk of liver damage and metabolic conditions like diabetes. More critically, for cognitive development, children who experience choline deficiency during key developmental stages may suffer impairments in mental function and overall cognitive performance, highlighting its importance from an early age (leading research, Harvard, 2024).
Given its critical role, it’s important to ensure adequate daily intake of choline. The recommended daily allowance is 550 mg for adult men and 425 mg for adult women over 19 years old. Dietary sources of choline are diverse and include:
- Animal Products: Meat, fish, dairy, and eggs are excellent sources.
- Plant-Based Foods: Whole grains, legumes (like soybeans and kidney beans), nuts, and seeds also contribute significantly.
- Vegetables and Fruits: Broccoli, cabbage, apples, and tangerines contain choline, though in smaller amounts.
Supplements are also available for those who struggle to meet their choline needs through diet alone. Ensuring a choline-rich diet is a proactive step towards supporting robust acetylcholine functions in the body and maintaining overall health.
5. When Acetylcholine Goes Wrong: Dysfunction and Health Impacts
The delicate balance of how acetylcholine functions in the body is critical for health, and disruptions can lead to significant physiological and neurological problems. Both a deficiency and an excess of this neurotransmitter can have damaging effects, impacting everything from muscle control to memory. Understanding these dysfunctions is crucial for recognizing and addressing related health conditions.
One of the most well-known conditions associated with acetylcholine deficiency is Alzheimer’s disease. While the exact causes of Alzheimer’s are complex and multi-faceted, a consistent finding is the significant loss of cholinergic neurons in the brain, leading to severely reduced acetylcholine levels (leading research, Harvard, 2024). This deficiency is strongly linked to the characteristic memory loss and cognitive decline seen in patients. Therapeutic strategies often involve medications designed to increase acetylcholine availability in the brain.
Conversely, excessive acetylcholine can also be detrimental, leading to a condition known as cholinergic crisis or toxicity. When acetylcholine accumulates excessively in synapses and neuromuscular junctions, it overstimulates receptors. Symptoms can include increased salivation, abdominal cramps, diarrhea, blurry vision, muscle twitches, and in severe cases, paralysis and respiratory failure. This can occur due to exposure to certain toxins or medications.
Myasthenia gravis is another autoimmune condition where the body’s immune system mistakenly attacks and damages acetylcholine receptors at the neuromuscular junction. This attack prevents acetylcholine from effectively stimulating muscle contraction, resulting in progressive muscle weakness that can affect the arms, legs, neck, and even muscles involved in breathing and swallowing. This highlights a problem not with acetylcholine production, but with its reception.
Parkinson’s disease, primarily known for dopamine deficiency, also involves acetylcholine imbalances. While dopamine loss in the substantia nigra is central, cholinergic overactivity in certain brain regions is believed to contribute to some motor symptoms, such as tremors and rigidity. Furthermore, exposure to certain toxins, such as nerve gases and some pesticides, can severely disrupt acetylcholine function by inhibiting the enzyme acetylcholinesterase, which breaks down ACh. This leads to a massive buildup of acetylcholine, causing symptoms of severe cholinergic toxicity and potentially death. Even natural toxins, like the venom from a black widow spider, cause an uncontrolled release of acetylcholine, leading to intense muscle contractions and paralysis. These examples underscore the critical importance of maintaining the precise balance of how acetylcholine functions in the body.
6. Modulating Acetylcholine: Therapeutic and Toxic Effects
Given acetylcholine’s profound influence on bodily functions, manipulating its activity is a key strategy in medicine and, unfortunately, in the realm of toxins. Medications are designed to either enhance or block acetylcholine’s actions, providing targeted treatments for various conditions. Conversely, certain substances can disrupt its delicate balance with severe, even fatal, consequences.
One well-known example of therapeutic modulation is Botox (botulinum toxin). This medication works by interfering with the release of acetylcholine at specific neuromuscular junctions where it is injected. By blocking ACh release, Botox causes localized muscle paralysis, which is why it’s effectively used to temporarily reduce wrinkles or treat conditions involving muscle spasms, such as chronic migraines or cervical dystonia. This demonstrates how precisely targeting how acetylcholine functions in the body can yield therapeutic benefits.
Another class of medications, known as AChE (acetylcholinesterase) inhibitors, are crucial for treating conditions like Alzheimer’s disease and myasthenia gravis. These drugs, including donepezil (Aricept), rivastigmine (Exelon), and galantamine (Razadyne), work by blocking the enzyme acetylcholinesterase, which is responsible for breaking down acetylcholine in the synaptic cleft. By inhibiting this enzyme, AChE inhibitors increase the amount of acetylcholine available to bind with receptors, thereby enhancing cholinergic signaling. This helps to improve cognitive symptoms in Alzheimer’s and muscle strength in myasthenia gravis.
Conversely, anticholinergics are medications that block the actions of acetylcholine by binding to its receptors. These drugs are often used in conditions where acetylcholine activity is excessive or needs to be reduced, such as in some forms of Parkinson’s disease to help manage tremors and rigidity. They can also be used to treat overactive bladder or certain types of muscle spasms. However, anticholinergics can have side effects like dry mouth, blurred vision, and cognitive impairment, especially in older adults, highlighting the complexity of modulating this neurotransmitter.
As of 2025, ongoing research continues to explore novel ways to modulate acetylcholine pathways, including gene therapies and more specific receptor-targeting drugs (leading research, Harvard, 2024). The goal is to develop treatments with fewer side effects and greater efficacy, further refining our ability to influence how acetylcholine functions in the body for improved health outcomes. However, the potent effects of acetylcholine also mean that toxins like nerve agents and certain pesticides deliberately target its pathways, leading to severe overstimulation and life-threatening cholinergic crises, underscoring the critical importance of its balanced regulation.
Results: Harnessing Your Body’s Chemical Messenger
Understanding how acetylcholine functions in your body provides invaluable insight into the intricate workings of your nervous system. From facilitating every muscle contraction to sharpening your memory and focus, this vital neurotransmitter is a cornerstone of both physical movement and cognitive ability. Recognizing its importance empowers you to make informed lifestyle choices that support its optimal function.
By ensuring adequate choline intake through a balanced diet, you directly support your body’s capacity to produce this essential chemical messenger. Awareness of symptoms related to acetylcholine imbalances can also prompt timely medical consultation, leading to early diagnosis and effective management of conditions like Alzheimer’s or myasthenia gravis. In essence, appreciating the role of acetylcholine is a step towards better self-care and a deeper connection with your body’s remarkable internal chemistry.