The human body is an intricate marvel, constantly performing countless functions without our conscious thought. From the steady rhythm of your heart to the subtle processes of digestion, an unseen conductor orchestrates these vital operations. This remarkable system is known as the autonomic nervous system (ANS), a crucial component of your peripheral nervous system. It’s responsible for regulating involuntary body functions, ensuring your internal environment remains stable, whether you’re relaxing or facing a sudden challenge. Understanding the ANS is key to appreciating how your body maintains balance and responds to the world around you, a concept increasingly relevant for holistic health in 2025 (Harvard, 2024).
Understanding the Autonomic Nervous System
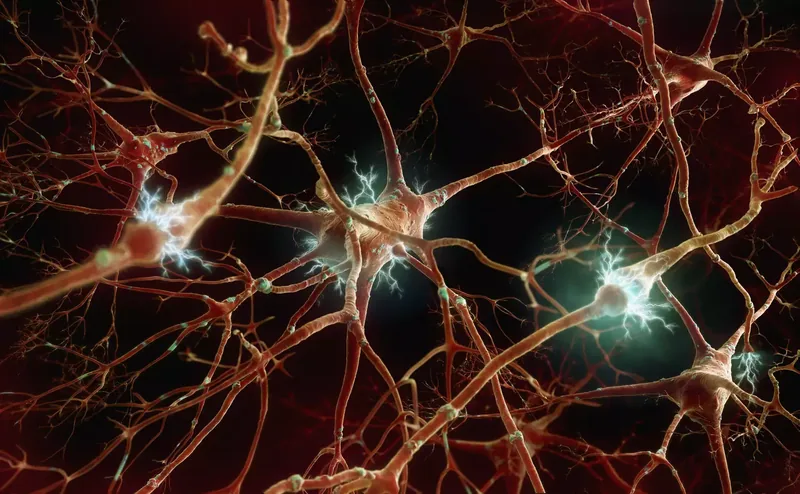
The autonomic nervous system (ANS) serves as the body’s internal control center, operating behind the scenes to maintain homeostasis. It’s a complex network of nerves that governs all the processes we don’t consciously think about, such as heartbeat, breathing, digestion, and blood pressure regulation. Often referred to as the involuntary nervous system, the ANS ensures our survival and adapts our internal state to external demands. This intricate system is a vital part of the peripheral nervous system, which connects the brain and spinal cord to the rest of the body.
The ANS gathers information from both our internal environment and external stimuli, processing it to initiate appropriate physiological responses. For instance, when you stand up quickly, the autonomic nervous system automatically adjusts blood flow to prevent dizziness. This constant, dynamic regulation highlights the ANS’s critical role in our daily well-being and overall health resilience. In 2025, a deeper understanding of the ANS is empowering individuals to take proactive steps in managing stress and promoting their physiological balance.
This sophisticated control system is further organized into three primary divisions: the sympathetic nervous system, the parasympathetic nervous system, and the enteric nervous system. Each branch plays a distinct yet interconnected role in managing the body’s vast array of functions. Together, they ensure that all involuntary processes run smoothly, adapting to our needs from moment to moment, whether we are resting, eating, or reacting to a perceived threat.
The Sympathetic and Parasympathetic Branches: A Balancing Act
The autonomic nervous system is famously characterized by its two primary branches that often work in opposition: the sympathetic and parasympathetic nervous systems. Think of them as the body’s accelerator and brake pedals, respectively. The sympathetic nervous system is primarily responsible for mobilizing the body for action, triggering what is commonly known as the “fight-or-flight” response. When activated, it rapidly prepares you to confront or flee from perceived threats, leading to physiological changes like an increased heart rate, dilated pupils to enhance vision, and the relaxation of bladder muscles. For example, if you suddenly encounter a barking dog, your sympathetic system will surge into action, pumping adrenaline and sharpening your senses.
Conversely, the parasympathetic nervous system is dedicated to “rest and digest” functions, promoting relaxation and conserving energy. After a stressful event, this system steps in to dampen the heightened responses, slowly returning the body to its normal, resting state. It slows your heart rate, constricts pupils, stimulates digestion, and promotes bladder control. An excellent example is how your body calms down after a workout or a stressful meeting, allowing you to recover and replenish resources. The parasympathetic system helps maintain normal bodily functions and conserves physical resources, ensuring long-term health and recovery.
These two branches work in a delicate, dynamic balance, constantly adjusting to the body’s needs and environmental cues. While traditionally the sympathetic system was associated with stimulation and the parasympathetic with inhibition, modern understanding reveals a more nuanced interplay. Both systems can exert stimulating or inhibiting effects depending on the target organ and the specific neurotransmitters involved. Their synchronized effort is crucial for maintaining physiological equilibrium, allowing the body to adapt effectively to a wide range of situations throughout your day.
The Enteric Nervous System: Your Gut’s Independent Brain
Beyond the well-known sympathetic and parasympathetic systems, the autonomic nervous system includes a third, often overlooked, yet incredibly vital division: the enteric nervous system (ENS). Sometimes referred to as the “second brain” or “gut brain,” the ENS is a complex network of neurons embedded in the walls of the gastrointestinal tract, extending from the esophagus to the anus. What makes the ENS particularly fascinating is its remarkable ability to operate largely independently of the brain and spinal cord, though it does communicate extensively with both. This semi-autonomous nature allows it to manage the intricate processes of digestion with impressive efficiency.
The primary role of the enteric nervous system is to control all aspects of the digestive process. This includes regulating the movement of food through the gut (peristalsis), controlling the secretion of enzymes and fluids essential for breaking down food, and managing blood flow within the gastrointestinal tract. For instance, the mere smell of food can activate your ENS, prompting your stomach to prepare for digestion by releasing gastric juices. This independent control ensures that digestion can proceed smoothly without requiring constant input from the central nervous system, freeing up cognitive resources for other tasks.
While independent, the ENS is not entirely isolated. It interacts closely with the sympathetic and parasympathetic systems, which can modulate its activity. For example, stress (a sympathetic response) can significantly impact gut function, leading to digestive issues. Conversely, a healthy gut contributes to overall well-being, highlighting the profound connection between digestive health and mental state. Research in 2025 continues to uncover the extensive role of the ENS in mood, immunity, and overall health, emphasizing the importance of gut health for holistic wellness (Harvard, 2024).
Key Functions Controlled by the Autonomic Nervous System
The autonomic nervous system is the silent orchestrator behind virtually every involuntary physiological process that keeps us alive and functioning. Its comprehensive control extends across numerous internal organs and systems, ensuring that our bodies adapt seamlessly to changing conditions. This intricate network regulates critical functions such that we rarely have to consciously intervene. Without the ANS, maintaining even basic life processes would be an overwhelming and impossible task.
Key functions under the ANS’s command include:
- Cardiovascular Regulation: Managing heart rate and blood pressure is a prime responsibility of the autonomic nervous system. It ensures that blood flow is appropriately distributed to different organs based on immediate needs, whether you’re resting or exercising.
- Respiratory Control: While breathing can be conscious, the ANS maintains your respiratory rate and depth automatically, adjusting it to oxygen demands and carbon dioxide levels.
- Digestion and Metabolism: From the moment food enters your mouth, the ANS controls salivation, enzyme secretion, gut motility, and nutrient absorption. It also influences metabolic rate and liver function.
- Temperature Regulation: The ANS manages body temperature by controlling sweating, blood flow to the skin, and even the tiny muscles that cause goosebumps when you’re cold (a process called piloerection).
- Fluid and Electrolyte Balance: It plays a role in kidney function, influencing urine production and the balance of essential electrolytes in the body.
- Pupillary Response: The ANS adjusts the size of your pupils in response to light levels, ensuring optimal vision, such as dilating in dim light to let in more light, or constricting in bright light to protect the eyes.
- Sexual Response: Various stages of sexual arousal and function are also governed by the involuntary nervous system.
- Immune System Modulation: Emerging research in 2025 suggests a significant link between the ANS and immune system activity, showing how stress (ANS activation) can influence inflammatory responses and disease susceptibility.
- Glandular Secretions: The ANS controls the production of various body fluids, including sweat, tears, and saliva, which are crucial for protection, lubrication, and digestion.
These diverse functions highlight the indispensable role of the autonomic nervous system in maintaining the body’s intricate internal balance and enabling us to thrive in different environments.
Neurotransmitters: The Chemical Messengers of the ANS
Communication within the autonomic nervous system relies heavily on specialized chemical messengers known as neurotransmitters. These substances are released by nerve cells and travel across synapses to transmit signals to target organs or other nerve cells. They are fundamental to how the sympathetic and parasympathetic systems exert their often opposing, yet coordinated, effects. Understanding these chemical signals provides deeper insight into how the body’s internal control center operates at a molecular level.
The two most prominent neurotransmitters in the autonomic nervous system are acetylcholine and norepinephrine.
- Acetylcholine: This neurotransmitter is a primary player, particularly within the parasympathetic nervous system. It often has an inhibiting effect, promoting “rest and digest” responses. For instance, acetylcholine is released at nerve endings to slow the heart rate, stimulate digestive processes, and constrict the pupils. It also plays a crucial role in the enteric nervous system, helping to regulate gut motility and secretions. In some sympathetic pathways, such as those controlling sweat glands, acetylcholine also has a stimulating effect, showcasing its versatility.
- Norepinephrine: Predominantly active within the sympathetic nervous system, norepinephrine (also known as noradrenaline) is largely responsible for stimulating the “fight-or-flight” responses. When released, it increases heart rate and blood pressure, dilates pupils, and diverts blood flow to muscles in preparation for action. It works alongside adrenaline (epinephrine), a hormone released by the adrenal glands, to amplify these stress responses throughout the body.
The precise balance and timing of these neurotransmitter releases dictate the body’s physiological state. For example, during a moment of intense focus or perceived danger, a surge of norepinephrine mobilizes your resources, while after a relaxing meal, acetylcholine helps settle your system. Disruptions in the production, release, or reception of these critical neurotransmitters can lead to various autonomic disorders, underscoring their vital role in maintaining the delicate equilibrium of the involuntary nervous system. Advances in neuroscience in 2025 are continually refining our understanding of these complex chemical interactions and their impact on health.
Decoding Autonomic Disorders (Dysautonomia)
When the delicate balance of the autonomic nervous system is disrupted, individuals can experience a range of conditions collectively known as autonomic disorders, or dysautonomia. These disorders occur when the sympathetic and parasympathetic components become out of sync, leading to a wide array of symptoms affecting various bodily functions. Because the ANS controls so many involuntary processes, dysautonomia can manifest in diverse and often challenging ways, making diagnosis complex. These conditions can significantly impact quality of life, transforming routine daily activities into struggles.
There are numerous types of autonomic disorders, each presenting with unique characteristics:
- Orthostatic Hypotension (OH): A common form where blood pressure drops suddenly upon standing, leading to dizziness, light-headedness, and even fainting. It’s often linked to other conditions like diabetes.
- Postural Orthostatic Tachycardia Syndrome (POTS): Characterized by an abnormal increase in heart rate upon standing, accompanied by symptoms like dizziness, fatigue, and brain fog, despite blood pressure remaining stable.
- Pure Autonomic Failure (PAF): A progressive neurodegenerative condition specifically affecting the peripheral autonomic nervous system, causing severe orthostatic hypotension and other autonomic dysfunctions.
- Multiple System Atrophy (MSA): A rare, progressive neurodegenerative disorder impacting movement, balance, and autonomic functions, often leading to fainting spells and bladder control issues.
- Familial Dysautonomia (Riley-Day Syndrome): A genetic disorder primarily affecting individuals of Ashkenazi Jewish descent, impacting nerve cell development and causing problems with digestion, tear production, and blood pressure.
- Acute Autonomic Paralysis: Often triggered by spinal cord injuries, particularly in the upper back, leading to dangerous fluctuations in blood pressure and heart rate.
- Postprandial Hypotension: An excessive drop in blood pressure occurring after eating a meal, which can result in dizziness, fainting, and falls.
These disorders can arise independently or as complications of other health conditions that damage the autonomic nervous system. Factors such as aging, chronic diseases like diabetes or Parkinson’s, autoimmune disorders, certain cancers, spinal cord injuries, and even alcohol or drug abuse can contribute to the development of dysautonomia. Recognizing the potential causes and diverse manifestations of these conditions is the first step toward effective management and improving patient outcomes in 2025.
Recognizing and Managing Autonomic Disorder Symptoms
Living with an autonomic disorder can be profoundly challenging, as symptoms are often varied, unpredictable, and can significantly impact daily life. Because the autonomic nervous system regulates so many diverse bodily functions, the manifestations of dysautonomia can be widespread, sometimes making them difficult to connect to a single underlying cause. Individuals may experience a fluctuating cluster of symptoms, which can be fleeting or triggered by specific situations, such as standing up quickly or after certain meals. This variability often complicates self-assessment and diagnosis.
Common symptoms that may indicate a disruption in the autonomic nervous system include:
- Cardiovascular Issues: Persistent dizziness, light-headedness, or even fainting spells upon standing (orthostatic hypotension), or a rapid heart rate (tachycardia) that feels disproportionate to activity.
- Gastrointestinal Problems: Chronic nausea, bloating, constipation, diarrhea, or difficulty emptying the stomach (gastroparesis), which can lead to significant discomfort and nutritional deficiencies.
- Thermoregulation Abnormalities: Profuse sweating or, conversely, a complete lack of sweat (anhidrosis), making it difficult for the body to regulate temperature effectively.
- Urinary and Sexual Dysfunction: Difficulty emptying the bladder, urinary incontinence, or erectile dysfunction, which can impact personal health and relationships.
- Fatigue and Cognitive Impairment: Persistent fatigue, brain fog, difficulty concentrating, or a general sense of inertia, severely affecting productivity and mental clarity.
- Sensory and Pain Issues: Numbness, tingling, or unexplained aches and pains, signaling potential nerve damage or dysfunction.
- Pupillary Abnormalities: A lack of normal pupillary response to light changes, indicating impaired neurological control over the eyes.
If you or someone you care about experiences a persistent combination of these symptoms, it is crucial to seek medical evaluation. Early recognition is key to managing these complex conditions. While there’s often no “cure” for many autonomic disorders, effective management strategies focus on alleviating symptoms and improving quality of life. This can involve lifestyle adjustments, medication, and therapies tailored to the specific type and severity of dysautonomia. A proactive approach to understanding and addressing these symptoms is vital for maintaining wellness in 2025.
Diagnosis and Treatment Approaches for ANS Conditions
Diagnosing conditions related to the autonomic nervous system can be notoriously complex, often requiring a patient and persistent approach from both the individual and their healthcare provider. Due to the widespread and often vague nature of symptoms, initial physical examinations and routine laboratory tests may appear normal, leading to frustration and delayed diagnosis. The key is to find a healthcare provider, ideally a neurologist or a specialist in autonomic disorders, who is knowledgeable and willing to conduct a thorough investigation, rather than dismissing symptoms as psychosomatic.
The diagnostic process typically involves a combination of specialized tests designed to assess various autonomic functions:
- Orthostatic Blood Pressure and Heart Rate Monitoring: Measuring blood pressure and heart rate while lying down, sitting, and standing helps identify conditions like orthostatic hypotension or POTS.
- Tilt Table Test: This test involves lying on a table that slowly tilts upright, while blood pressure and heart rate are continuously monitored, to reproduce symptoms of orthostatic intolerance.
- Quantitative Sudomotor Axon Reflex Test (QSART): This evaluates the integrity of the sweat-producing nerves, assessing the body’s ability to regulate temperature.
- Valsalva Maneuver: This involves forced exhalation against a closed airway, which tests cardiovascular autonomic reflexes by observing changes in heart rate and blood pressure.
- Electrocardiogram (ECG): To assess heart rhythm and rule out other cardiac issues.
- Pupillary Light Reflex Test: To evaluate the autonomic control over pupil size and reactivity.
While there is currently no single “cure” for most autonomic disorders, treatment focuses on managing symptoms and addressing any underlying conditions. Strategies often include:
- Lifestyle Modifications: These are often the first line of defense. They include increasing fluid and salt intake (for hypotension), wearing compression garments, regular moderate exercise, avoiding triggers like sudden standing, and eating smaller, more frequent meals.
- Medications: Depending on the specific symptoms, medications may be prescribed to regulate blood pressure, heart rate, digestion, or other affected functions.
- Treating Underlying Conditions: Managing conditions like diabetes, autoimmune diseases, or Parkinson’s disease is crucial, as they can significantly impact autonomic nerve function.
- Physical Therapy and Occupational Therapy: To help improve mobility, balance, and daily functioning.
- Mental Health Support: Addressing anxiety and depression, which can be both symptoms and exacerbating factors of autonomic disorders.
Proactive health measures can also help prevent or mitigate the risk of developing autonomic nervous system conditions. These include maintaining a healthy diet to avoid nutritional deficiencies, engaging in regular physical activity, avoiding substance misuse, and promptly treating chronic health conditions that can affect autonomic nerves. Continued research in 2025 aims to uncover more targeted therapies and preventative strategies for these complex conditions.