The journey to overcoming opioid use disorder (OUD) often involves medications like Suboxone (buprenorphine/naloxone), a crucial tool for many. While highly effective, the thought of discontinuing Suboxone can bring apprehension, particularly regarding the duration and intensity of withdrawal from Suboxone. Understanding what to expect is the first step toward a successful transition. Typically, acute Suboxone withdrawal symptoms last about one week, though some psychological discomfort can linger longer. It’s paramount to approach cessation under medical supervision to minimize symptoms and ensure safety.
Navigating the process of ending Suboxone treatment requires careful planning and support. Abruptly stopping, often called “cold turkey,” can trigger significant withdrawal symptoms, making the process unnecessarily difficult and increasing the risk of relapse. Your doctor can guide you through a safe tapering schedule, which gradually reduces your dose over time, making withdrawal from Suboxone much more manageable. This comprehensive guide will illuminate the timeline, symptoms, coping mechanisms, and long-term strategies for a successful recovery journey in 2025 and beyond.
1. Understanding Suboxone and Withdrawal
Suboxone, a combination of buprenorphine and naloxone, plays a pivotal role in treating opioid use disorder (OUD) by reducing cravings and withdrawal symptoms without producing the intense “high” associated with full opioids. Buprenorphine is a partial opioid agonist, meaning it activates opioid receptors but to a lesser degree than full agonists like heroin or fentanyl. Naloxone, an opioid antagonist, is included to deter misuse; if injected, it blocks opioid effects, potentially triggering immediate withdrawal. This dual action makes Suboxone a cornerstone of medication-assisted treatment (MAT) for many individuals striving for recovery.
Despite its benefits, it’s crucial to recognize that buprenorphine is still an opioid, and consequently, your body will develop a physical dependence on it. This means that if you attempt to stop taking Suboxone suddenly, you will inevitably experience withdrawal from Suboxone. The body, accustomed to the presence of the medication, reacts to its absence with a range of physical and psychological symptoms. This isn’t a sign of addiction in the traditional sense when used as prescribed, but rather a physiological adjustment. Understanding this distinction is vital for anyone preparing to discontinue treatment, as it frames withdrawal as a natural, albeit uncomfortable, biological process that can be managed effectively with proper medical guidance.
Approaching Suboxone withdrawal with a clear understanding of its nature and the importance of medical supervision is key to a successful outcome. The goal is not merely to stop the medication but to transition safely and sustainably into a life free from opioid dependence. Medical professionals can help devise a personalized tapering plan, mitigating the severity of symptoms and providing necessary support. As treatment protocols continue to evolve in 2025, the emphasis remains on patient-centered care, ensuring that individuals feel empowered and supported throughout their journey to discontinuing Suboxone.
2. The Suboxone Withdrawal Timeline: What to Expect
The duration of withdrawal from Suboxone is a primary concern for anyone considering cessation. While individual experiences can vary, acute Suboxone withdrawal symptoms typically last for about a week, though some may persist for up to 10 days. Unlike short-acting opioids, Suboxone’s long half-life means that withdrawal symptoms often take longer to appear, usually beginning two to four days after the last dose. This delayed onset can sometimes catch individuals off guard if they are not prepared.
What is the typical Suboxone withdrawal timeline? Suboxone withdrawal symptoms generally begin within 2-4 days after the last dose, peak around days 3-5, and largely resolve within 7-10 days. However, certain psychological symptoms can linger for several weeks.
The peak intensity of symptoms typically occurs around days three to five. During this period, both physical and psychological discomfort tend to be at their highest. For instance, muscle aches and joint pain might start to subside after the first 72 hours, offering some relief. However, feelings of restlessness and anxiety can be more enduring, potentially lasting for a full week or even longer for some individuals. Other common physical symptoms, such as a runny nose or congestion, usually disappear within 10 days. It is important to note that while acute physical symptoms usually resolve within this timeframe, a general sense of unease or persistent opioid cravings can extend for a few months, necessitating continued support and strategies for managing these feelings (Harvard, 2024).
Planning for this timeline with your healthcare provider is essential. A gradual tapering schedule, where your dose is slowly reduced over time, can significantly soften the impact of these symptoms. This controlled approach allows your body to adjust more gently to lower levels of the medication, making the overall withdrawal from Suboxone experience less distressing. Open communication with your doctor about your experiences during the taper can help them adjust the schedule to your specific needs, ensuring the most comfortable and effective transition possible.
3. Navigating Suboxone Withdrawal Symptoms
When undergoing withdrawal from Suboxone, individuals can anticipate a range of both physical and psychological symptoms. These symptoms arise as the body adjusts to the absence of the medication it has become dependent on. While Suboxone is designed to be less severe in its withdrawal profile compared to full opioid agonists, discontinuing it without proper tapering will still lead to noticeable discomfort. Recognizing these symptoms is the first step toward managing them effectively and understanding the importance of medical supervision.
Physical Symptoms of Suboxone Withdrawal
The physical manifestations of Suboxone withdrawal often mirror those of a severe cold or flu. These can include:
- Chills and Goose Bumps: Often referred to as “cold turkey,” these sensations are common as the body’s temperature regulation is affected.
- Muscle Aches and Pains: Widespread discomfort in muscles and joints is a hallmark symptom, sometimes described as a deep, aching sensation.
- Nausea or Vomiting: Gastrointestinal distress is frequent, potentially leading to nausea, stomach cramps, and diarrhea.
- Runny Nose and Teary Eyes: These “cold-like” symptoms are part of the body’s autonomic nervous system response.
- Sweating: Excessive sweating, particularly at night, can occur.
- Tremors or Twitching: Involuntary muscle movements can range from mild tremors to more pronounced twitching.
For individuals who previously struggled with more potent opioid addictions, the physical withdrawal from Suboxone should ideally be less intense than their past experiences. Healthcare professionals use tools like the Clinical Opiate Withdrawal Scale (COWS) to objectively assess symptom severity, helping tailor treatment and support during this phase.
Psychological Symptoms of Suboxone Withdrawal
Beyond the physical, the psychological impact of withdrawal from Suboxone can be profoundly challenging. These symptoms include:
- Anxiety: A heightened sense of worry, nervousness, or panic is very common.
- Depression: Feelings of sadness, hopelessness, and a lack of motivation can emerge or intensify.
- Restlessness: An inability to sit still or a constant urge to move, often accompanied by irritability.
- Anhedonia: A temporary inability to feel pleasure, which can make daily activities seem dull or unrewarding.
It’s important to differentiate between withdrawal-induced psychological symptoms and the re-emergence of underlying mental health conditions. Suboxone withdrawal can sometimes unmask or exacerbate pre-existing anxiety or depression that was previously muted by drug use. Furthermore, the emotional weight of confronting past behaviors related to addiction can lead to feelings of guilt and regret. This complex interplay underscores why robust psychological support, including counseling and therapy, is indispensable during and after the acute phase of withdrawal from Suboxone. Seeking help for these emotional challenges is not a sign of weakness but a critical component of holistic recovery.
4. Effective Strategies for Coping and Tapering
Successfully navigating withdrawal from Suboxone largely depends on a well-structured tapering plan developed in close collaboration with your doctor. Tapering means gradually reducing your Suboxone dose over time, allowing your body to adjust slowly and minimizing the severity of withdrawal symptoms. This controlled approach is the gold standard for discontinuing the medication and significantly improves the chances of a smooth transition.
The Importance of a Tapering Schedule
Suboxone tapering schedules can vary widely, typically ranging from 7 to 28 days, though some individuals may benefit from an even longer, more gradual reduction. Research has shown mixed results regarding the ideal taper length; some studies suggest that shorter, seven-day tapers can be successful for certain populations, particularly when tightly monitored (Harvard, 2024). However, many experts advocate for a slow, flexible tapering schedule. This allows your doctor to adjust the pace of dose reduction based on your individual experience, slowing down if you encounter uncomfortable symptoms and ensuring you remain as comfortable as possible throughout the process.
Can I taper Suboxone on my own? Attempting to taper Suboxone without medical supervision is strongly discouraged. Self-tapering significantly increases the risk of failure, severe withdrawal symptoms, and potential relapse, making the recovery journey much harder.
It’s crucial to resist the temptation to self-taper, especially if you’re feeling isolated or have acquired Suboxone illicitly. Unsuccessful attempts to quit can be incredibly discouraging and emotionally taxing, potentially setting back your recovery efforts. Always work with a qualified healthcare professional who can provide the necessary medical oversight, prescribe supportive medications, and offer psychological guidance throughout your withdrawal from Suboxone.
Supportive Medications and Lifestyle Adjustments
Even with a careful taper, some individuals may still experience breakthrough withdrawal symptoms. In such cases, your doctor might recommend additional medications to help manage specific discomforts. Lucemyra (lofexidine hydrochloride), approved by the FDA in 2018, is a notable non-opioid option specifically designed to treat opioid withdrawal symptoms by reducing the release of norepinephrine, a neurotransmitter linked to withdrawal. This medication can be initiated immediately after your last Suboxone dose and is typically used for up to 14 days.
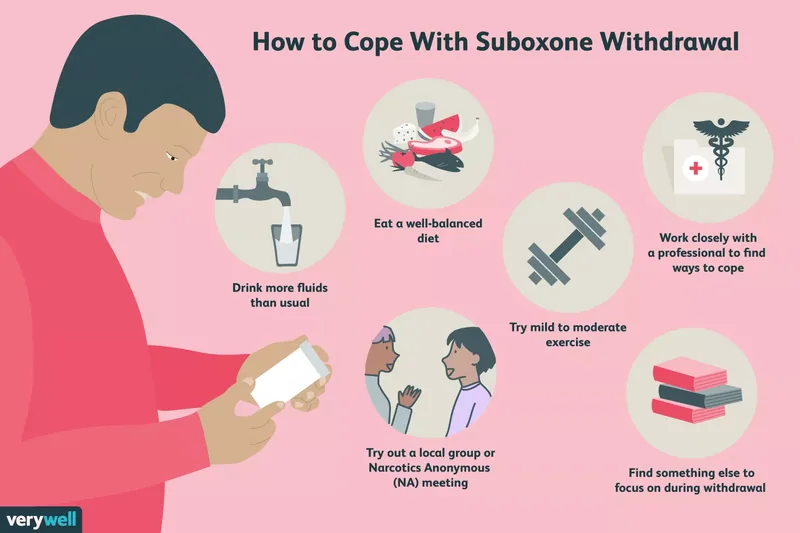
Beyond medication, integrating certain lifestyle changes can significantly aid in coping with Suboxone withdrawal. Staying well-hydrated by drinking plenty of fluids is essential to prevent dehydration, which can worsen symptoms. Maintaining a balanced diet helps replenish vital vitamins and electrolytes, supporting overall body function. Engaging in mild to moderate exercise, such as walking or gentle yoga, can alleviate restlessness and improve mood. Practicing relaxation techniques like meditation, deep breathing exercises, or listening to calming music can help manage anxiety and agitation. Finally, finding distractions through hobbies, books, or television can shift focus away from discomfort. Seeking support from community groups, therapy, or Narcotics Anonymous (NA) meetings provides invaluable encouragement and shared experience, reinforcing your commitment to successfully completing withdrawal from Suboxone.
5. Addressing Relapse Risk and Long-Term Recovery
While withdrawal from Suboxone is generally not life-threatening, unlike acute withdrawal from some full opioid agonists, the period immediately following cessation carries a significant risk: relapse. Opioid withdrawal, even when managed with a taper, can be intensely unpleasant, and the desire to alleviate discomfort can be a powerful trigger for returning to drug use. For individuals who have been on Suboxone, this risk is particularly concerning because their opioid tolerance will have substantially decreased.
Why is relapse dangerous after Suboxone withdrawal? Relapsing after Suboxone withdrawal is highly dangerous because your opioid tolerance will have significantly decreased. Using the same amount of opioids as before can lead to a severe, potentially fatal overdose due to respiratory depression.
A relapse at this stage can be devastating, not only psychologically but also physically. Your body will no longer be accustomed to the same opioid doses you might have used previously. This reduced tolerance means that even a seemingly small amount of opioids can lead to a dangerous or fatal overdose. Therefore, it is absolutely critical to work closely with medical professionals throughout your Suboxone taper and to have a robust relapse prevention plan in place. This plan should include immediate access to support systems and, if applicable, overdose reversal medication like naloxone.
Building a Strong Long-Term Treatment Plan
Successfully completing withdrawal from Suboxone marks a monumental achievement, but it’s just one phase of a lifelong recovery journey. The physical dependence on opioids may be broken, but the psychological aspects of addiction often require continued attention. A comprehensive long-term treatment plan is essential for preventing future relapse and fostering sustained well-being.
Talk therapy plays a pivotal role in this long-term strategy. Through individual or group counseling, you can explore the underlying reasons for your initial drug use, identify personal triggers, and develop healthier coping mechanisms. Cognitive Behavioral Therapy (CBT), for example, helps individuals recognize and challenge negative thought patterns that can lead to poor decision-making and drug use. Learning to manage stress, identify high-risk situations, and develop refusal skills are all critical components of relapse prevention (Harvard, 2024). Research consistently demonstrates that combining talk therapy with medication management (even after Suboxone cessation, through other non-opioid medications if needed) is more effective for treating opioid addiction than medication alone, highlighting the importance of integrated care in 2025.
Whether you choose one-on-one sessions with a psychologist, participate in group therapy at a community clinic, or engage with addiction counselors, consistent psychological support is a cornerstone of recovery. This ongoing engagement helps solidify the gains made during withdrawal from Suboxone and equips you with the tools necessary to navigate life’s challenges without resorting to substance use.
6. Special Considerations: Pregnancy and Support
The decision to discontinue Suboxone, or to adjust treatment, often involves unique circumstances that require careful medical consideration. One of the most significant special considerations is pregnancy, where the health of both the mother and the developing fetus must be prioritized. If you are pregnant or breastfeeding and considering changes to your Suboxone regimen, immediate consultation with a healthcare professional is non-negotiable.
Quitting Suboxone During Pregnancy
While Suboxone (buprenorphine/naloxone) is generally not recommended during pregnancy due to the naloxone component, buprenorphine without naloxone is often deemed safe and effective for treating OUD in pregnant individuals. Depending on your specific situation, your doctor may recommend several approaches:
- Accelerated Taper: A carefully monitored, faster reduction of Suboxone, if medically appropriate and safe for both mother and baby.
- Switch to Buprenorphine Monotherapy: Transitioning to buprenorphine-only medication, which has a well-established safety profile during pregnancy and can prevent neonatal abstinence syndrome (NAS) or make it less severe.
- Switch to Methadone: Methadone is another well-researched and proven safe medication for OUD during pregnancy, often utilized in specialized treatment programs.
The goal is to maintain stability and prevent relapse, which can be far more dangerous for both mother and baby than continuing prescribed medication. Decisions around medication for OUD during pregnancy are complex and require a multidisciplinary team approach to ensure the best possible outcomes (Harvard, 2024). Never attempt to stop withdrawal from Suboxone or any OUD medication independently if you are pregnant or breastfeeding.
Finding Support for Your Recovery Journey
Regardless of your specific circumstances, a robust support system is vital for anyone undergoing withdrawal from Suboxone and embarking on long-term recovery. You don’t have to face this journey alone.
- Medical Team: Your doctor, addiction specialist, and therapists are your primary resources for safe tapering, symptom management, and psychological support.
- Family and Friends: Enlisting the understanding and encouragement of loved ones can provide emotional strength and practical help. Educate them about what you’re experiencing so they can better support you.
- Support Groups: Organizations like Narcotics Anonymous (NA) offer invaluable peer support, a sense of community, and a structured approach to recovery. Hearing from others who have successfully navigated withdrawal from Suboxone and sustained sobriety can be incredibly motivating.
- Community Resources: Many local clinics and mental health centers offer group therapy, individual counseling, and case management services tailored to addiction recovery.
If you or a loved one are struggling with substance use or addiction, please reach out for help. The Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357 provides confidential information on support and treatment facilities in your area. Taking this crucial step is a testament to your commitment to health and well-being, paving the way for a successful future beyond withdrawal from Suboxone.