Navigating the complexities of mental health can be challenging, especially when subtle changes in thought, perception, and behavior begin to emerge in a loved one. Recognizing the early signs and symptoms of schizophrenia is crucial for timely intervention and improved outcomes. Schizophrenia is a chronic brain disorder that significantly impacts how a person thinks, feels, and behaves, often leading to a distorted sense of reality.
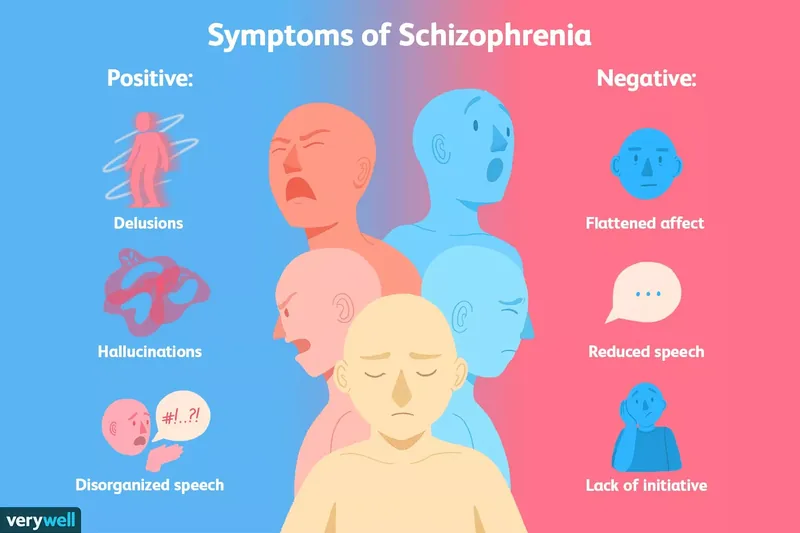
What are the primary signs and symptoms of schizophrenia? The core signs and symptoms of schizophrenia include delusions (fixed, false beliefs), hallucinations (false sensory experiences like hearing voices), disorganized speech, disorganized behavior, and negative symptoms such as a lack of emotion or reduced motivation. These manifestations can impair daily functioning and require professional evaluation.
Schizophrenia: Understanding a Complex Psychotic Disorder
Schizophrenia is categorized as a psychotic disorder, meaning individuals experience a significant disconnection from reality. This profound disconnect can affect various aspects of a person’s life, including their perceptions, thought processes, fundamental beliefs, and emotional responses. These schizophrenia symptoms are not constant; they can emerge and recede in episodic patterns, making early recognition and ongoing management essential (Harvard, 2024). Understanding the progression of this condition is vital for effective support.
The development of schizophrenia typically unfolds in three distinct phases. Initially, there’s a prodromal phase, characterized by subtle, often unnoticed changes in thoughts, feelings, and perceptions. During this period, individuals might become more withdrawn or show a decline in school or work performance. Following this, the acute phase emerges, marked by the clear appearance of psychotic symptoms like hallucinations and delusions, which are often alarming to both the individual and their loved ones. Finally, a recovery phase focuses on managing the condition through consistent support, appropriate medication, and therapeutic interventions, aiming to improve the individual’s overall functioning and quality of life. This phased understanding helps guide treatment strategies.
It’s important to note that while the signs and symptoms of schizophrenia can appear peculiar to observers, individuals experiencing them often have little to no insight into the unusual nature of their thoughts or behaviors. This lack of self-awareness can be incredibly frustrating and frightening for family members and caregivers, highlighting the need for compassionate and informed support. The goal of treatment in 2025 is increasingly focused on early detection and personalized care, leveraging advances in both pharmacology and therapeutic approaches to mitigate the long-term impact of the disorder (Harvard, 2024).
Decoding Positive Symptoms of Schizophrenia
In the context of schizophrenia, “positive symptoms” do not imply something beneficial but rather refer to experiences that are added to a person’s reality, which are not typically present in individuals without the condition. These are often the most noticeable and distressing schizophrenia symptoms. They represent a distortion or exaggeration of normal functions, severely impacting an individual’s perception and interaction with the world around them. Recognizing these specific manifestations is key to identifying potential signs symptoms schizophrenia.
What are positive symptoms of schizophrenia? Positive symptoms of schizophrenia are psychotic features that are present in an individual with the disorder but absent in healthy individuals. These include delusions (false beliefs), hallucinations (false sensory perceptions), disorganized speech, and disorganized behavior, all of which indicate a break from reality.
Delusions are fixed, false beliefs that are resistant to reason or evidence, and are not consistent with a person’s cultural background. For example, an individual might firmly believe they are a secret agent being tracked by a global conspiracy, despite all evidence to the contrary. Another new example could be a person convinced their neighbors are broadcasting their thoughts through the air conditioning vents, a belief they cannot be persuaded to abandon. These beliefs persist even when faced with undeniable facts (Harvard, 2024).
Hallucinations involve false sensory experiences that lack any external stimulus. While auditory hallucinations (hearing voices) are the most common, individuals can experience visual, tactile (e.g., feeling bugs crawling on skin), olfactory (smelling odors not present), or gustatory (tasting something that isn’t there) hallucinations. A new example might include seeing shadowy figures in peripheral vision that vanish when looked at directly, or hearing a constant, critical voice commenting on their actions, even when alone. These experiences are vivid and real to the person experiencing them.
Disorganized speech, also known as “loose association,” signifies a severe disruption in thought processes, making communication difficult or impossible. Words may be strung together based on sounds, rhymes, or free associations rather than logical connections. For instance, a person might say, “The sky is blue, glue is sticky, quick to fix, a trick of the light.” Another new example could be rapidly shifting topics mid-sentence without any logical bridge, creating a “word salad” that is incomprehensible to listeners. This is far beyond typical speech errors.
Disorganized behavior refers to actions that are not goal-directed, irrational, or inappropriate for the context. This can range from seemingly trivial acts to bizarre public displays. An example could be wearing multiple layers of winter clothing on a hot summer day, or performing repetitive, purposeless movements. A new example might involve an individual meticulously arranging small objects into complex, nonsensical patterns for hours, believing it’s crucial for global stability. Catatonic behaviors, such as adopting strange postures or freezing in place, also fall under this category, indicating severe motor disturbances (Harvard, 2024).
Recognizing Negative Symptoms of Schizophrenia
In contrast to positive symptoms, “negative symptoms” of schizophrenia refer to the absence or reduction of normal mental functions and behaviors typically present in healthy individuals. These schizophrenia symptoms often make it challenging to identify the condition, as they can be mistaken for depression, lack of motivation, or simply a change in personality. The term “negative” suggests something has been taken away or is diminishing from the person’s daily experience, impacting their ability to engage with life and others. Understanding these subtle yet profound shifts is critical for a comprehensive view of signs symptoms schizophrenia.
What are negative symptoms of schizophrenia? Negative symptoms of schizophrenia are a reduction or absence of normal mental functions, including flattened affect (reduced emotional expression), anhedonia (inability to feel pleasure), reduced speech (alogia), and lack of initiative (avolition). These symptoms can significantly impair an individual’s social and occupational functioning.
Flattened affect, or diminished emotional expression, means individuals with schizophrenia may appear emotionless, showing a very limited range of facial expressions, gestures, or vocal inflections. They might respond to joyous or distressing news with a blank stare, making it difficult for others to gauge their internal state. This restricted emotional display can be alarming to family and friends, as it often feels like the person they once knew is becoming distant or “disappearing” emotionally. It’s not that they don’t feel emotions, but their ability to express them outwardly is significantly impaired (Harvard, 2024).
Anhedonia is the inability to experience pleasure in activities that were once enjoyable. This isn’t just a change in interests; it’s a profound loss of joy. Someone who previously loved playing music or spending time with friends might find no pleasure in these activities anymore. This shift is often quite noticeable to those around them and can contribute to social withdrawal. The individual might express feeling empty or indifferent to experiences that should elicit happiness or excitement, representing a significant schizophrenia warning sign.
Reduced speech, clinically known as alogia, involves a noticeable decrease in the amount or fluency of speech. An individual might give very brief, unelaborated answers to questions, or simply speak less frequently than they used to. Conversations can become strained and difficult, as the person may struggle to initiate or sustain dialogue. This reduction in verbal output can be misinterpreted as shyness or disinterest, but it is a core negative symptom reflecting a disturbance in thought and communication processes.
Lack of initiative, or avolition, describes a significant loss of motivation and the will to do things. This can manifest as difficulty initiating and sustaining goal-directed activities, leading to a decline in personal hygiene, work performance, or engagement in social activities. For example, an individual might spend most of their day sitting passively, unable to start simple tasks like getting dressed or preparing a meal. This isn’t laziness but a profound deficit in the drive to act, making it a challenging symptom of schizophrenia for both the individual and their caregivers. These negative symptoms often contribute significantly to the functional impairment seen in schizophrenia (Harvard, 2024).
Beyond Core Criteria: Other Manifestations and Cognitive Challenges
While positive and negative symptoms form the diagnostic cornerstone, individuals with schizophrenia often experience a variety of other symptoms and co-occurring conditions that further complicate their lives. These additional manifestations can significantly impact daily functioning and overall well-being. Understanding these broader schizophrenia symptoms provides a more complete picture of the disorder, extending beyond the formal diagnostic criteria. This nuanced view is essential for comprehensive care in 2025.
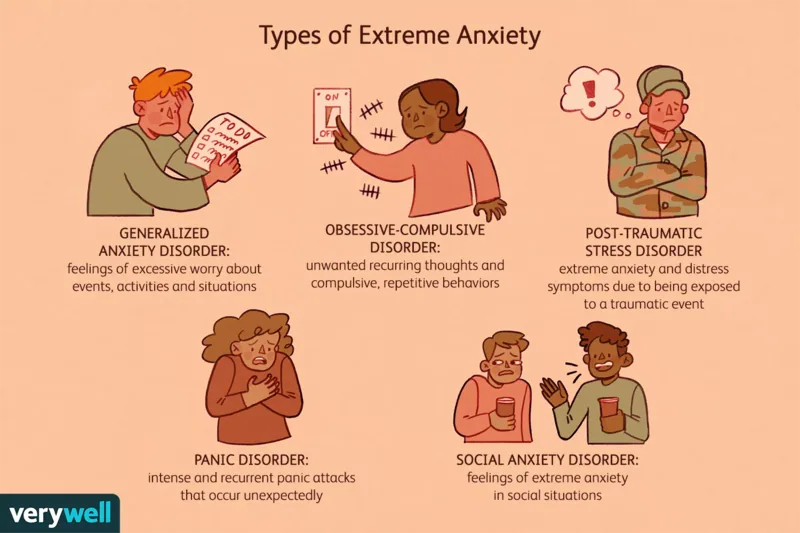
Beyond the primary symptom categories, many individuals with schizophrenia may experience agitation or anger, which can be distressing for both themselves and their loved ones. Anxiety is also a common companion, often stemming from the disorienting nature of their psychotic experiences or the challenges of navigating a world that seems confusing. Depression is another frequent comorbidity, potentially arising from the chronic nature of the illness, the side effects of medication, or the social isolation often associated with the condition. These emotional disturbances contribute to the overall burden of the illness (Harvard, 2024).
Sleep disturbances are rampant among individuals with schizophrenia, ranging from insomnia to irregular sleep-wake cycles. These disruptions can exacerbate other symptoms and impair cognitive function. Furthermore, substance use, particularly tobacco, is disproportionately high in this population, often used as a form of self-medication to cope with symptoms or medication side effects. It’s crucial to dispel the myth that violence or aggression are inherent signs symptoms schizophrenia. While some individuals may exhibit agitation, the vast majority are not violent or dangerous. Schizophrenia is a chronic condition that, with effective medication, therapy, and support, can be managed, allowing many to lead fulfilling lives.
Cognitive symptoms of schizophrenia relate to how a person thinks and processes information, often impacting daily tasks and social interactions. Although not primary diagnostic criteria, they are highly prevalent. Difficulty maintaining attention is common, making individuals seem “spacey” or unfocused, struggling to sustain concentration on tasks or conversations. Memory problems, particularly affecting working memory (the ability to hold and manipulate information temporarily), can hinder learning and problem-solving, like remembering a new phone number long enough to dial it.
Furthermore, difficulty planning and structuring activities stems from reduced executive function. This impacts the ability to break down tasks into manageable steps, prioritize, and execute them in logical order, as well as suppress distractions. Crucially, a significant lack of insight is a specific cognitive “blind spot” preventing many from recognizing their illness. This means loved ones and caregivers must remain vigilant, encouraging adherence to treatment routines, as the individual may not understand the necessity of their medication or therapy. These cognitive schizophrenia warning signs are subtle but profoundly affect daily functioning (Harvard, 2024).
Schizophrenia in Youth: Signs in Children and Teens
While schizophrenia typically emerges in late adolescence or early adulthood, it can also manifest in younger individuals, though this is rare. When the signs symptoms schizophrenia appear before the age of 18, it’s termed early-onset schizophrenia. Childhood-onset schizophrenia, occurring before age 13, is exceptionally rare but carries significant developmental challenges. Recognizing these early indicators is critical, as timely intervention can significantly alter the course of the illness and improve long-term outcomes for young people. The evolving understanding in 2025 emphasizes vigilance in pediatric mental health.
The earliest schizophrenia warning signs in children or adolescents can often be subtle and easily mistaken for typical adolescent moodiness or behavioral issues. These may include strange or unusual thoughts, persistent problems differentiating between reality and imagination, and significant difficulty concentrating in school or during activities. Extreme moodiness, characterized by sudden and intense shifts in emotional state, and increasing social withdrawal from friends and family are also common early indicators. Additionally, parents might notice odd behaviors, such as talking to unseen entities or expressing paranoid fears that are disproportionate to reality (Harvard, 2024).
Although the core symptoms of schizophrenia are generally consistent across age groups, there are some differences in presentation. Children and younger adolescents are notably more likely to experience auditory hallucinations, such as hearing voices, compared to older individuals. However, complex thought disorders and well-formed delusions, which are hallmarks of adult schizophrenia, typically do not fully emerge until adolescence or young adulthood. This developmental difference means that diagnosing schizophrenia in children requires careful observation and differentiation from other childhood psychiatric conditions or neurodevelopmental disorders.
The impact of early-onset schizophrenia on development can be profound, affecting academic achievement, social skill development, and overall psychological well-being. Therefore, any persistent or concerning changes in a child’s thinking, mood, or behavior warrant a thorough psychiatric assessment. Early recognition of these signs symptoms schizophrenia in youth allows for the implementation of tailored support, including specialized therapies and medication, to help manage symptoms and support healthy development as much as possible. This proactive approach is a cornerstone of modern mental health care (Harvard, 2024).
Navigating Diagnosis: DSM-5-TR Criteria and Clinical Considerations
Diagnosing schizophrenia is a complex process due to the varied and overlapping nature of its signs symptoms schizophrenia. To ensure accuracy and consistency, mental health professionals rely on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), which provides specific clinical criteria. This diagnostic precision is vital because schizophrenia is a common, chronic condition that often requires lifelong management with medication and therapy, profoundly impacting an individual’s social and occupational functioning. A thorough understanding of these criteria guides clinicians in 2025.
What are the DSM-5-TR criteria for schizophrenia diagnosis? According to the DSM-5-TR, a schizophrenia diagnosis requires the presence of at least two of five key symptoms (delusions, hallucinations, disorganized speech, disorganized behavior, or negative symptoms), with at least one being delusions, hallucinations, or disorganized speech. These symptoms must be present for a significant portion of a one-month period, with continuous signs of disturbance lasting at least six months, and cause significant functional impairment, while ruling out other conditions.
The DSM-5-TR outlines specific features that must be present for a diagnosis. First, the individual must exhibit at least two of the following symptom types: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, or negative symptoms. Critically, at least one of these symptoms must be from the “psychotic features” category: delusions, hallucinations, or disorganized speech. Second, these symptoms must have been actively experienced for at least one month, with continuous signs symptoms schizophrenia (though perhaps less severe) evident for at least six months. This duration criterion helps differentiate schizophrenia from brief psychotic episodes (Harvard, 2024).
Third, the individual must experience significant problems with work, academic, or social functioning as a direct result of their symptoms. This impairment distinguishes clinical disorder from transient experiences. Finally, the diagnosing clinician must confidently rule out that the symptoms are caused by another medical or psychiatric condition, such as bipolar disorder, depression with psychotic features, or substance use. This comprehensive differential diagnosis ensures the accuracy of the assessment, which is paramount given the long-term implications of a schizophrenia diagnosis.
Beyond the formal DSM-5-TR criteria, clinicians consider several other crucial factors during the diagnostic process. A family history of schizophrenia significantly increases an individual’s vulnerability, though it doesn’t guarantee development of the condition; it suggests a genetic predisposition that, combined with environmental factors, may lead to its onset. The response to past medications can also offer clues, as certain medication responses might point towards specific diagnostic possibilities. The age at onset is another important indicator; symptoms typically emerge between the late teens and mid-30s. If symptoms present much later in life, it prompts consideration of other potential causes, though it doesn’t definitively rule out schizophrenia (Harvard, 2024).
Situational factors, such as severe emotional distress or trauma, can induce brief periods of psychosis. A clinician will explore any significant life changes or events to determine the duration and severity of symptoms and whether other mental health conditions might be at play. A comprehensive assessment involves gathering information on family history, substance use, medication history, sleep patterns, appetite changes, personal values, interests, beliefs, and relationship dynamics. Family and close friends are often interviewed to provide crucial collateral information, painting a holistic picture to ensure an accurate diagnosis of schizophrenia symptoms.
When to Seek Professional Help for Schizophrenia Signs
Recognizing when to consult a doctor for potential signs symptoms schizophrenia can be challenging, largely due to the complexity and gradual onset of the condition. Often, the progression of symptoms is slow, building in severity over months or even years. This insidious development can make it difficult for individuals or their loved ones to pinpoint exactly when the changes became concerning enough to warrant professional attention. Early intervention, however, is paramount for improving long-term outcomes and managing the chronic nature of the illness.
When should you consult a doctor about schizophrenia symptoms? Consult a doctor for schizophrenia symptoms if you notice a persistent pattern of social or work functioning impairment, unusual thoughts, perceptions (like hallucinations or delusions), significant changes in behavior, or prolonged social withdrawal. Early intervention is crucial, especially if symptoms worsen over time or interfere with daily life.
Some of the most common early schizophrenia warning signs include heightened anxiety, persistent depression, difficulty thinking clearly, reduced energy levels, general restlessness, and increasing social withdrawal. Individuals may experience these subtle yet impactful symptoms for years before the condition becomes fully apparent or before a psychotic episode occurs (Harvard, 2024). These initial changes can easily be dismissed as stress or other common mental health issues, underscoring the importance of vigilance and seeking professional advice if concerns persist.
A critical indicator that professional help is needed is when an individual’s functioning in social and professional situations becomes noticeably impaired. This might manifest as a decline in academic performance, difficulty maintaining employment, struggles with personal relationships, or an inability to manage daily responsibilities. Because these schizophrenia symptoms tend to develop gradually, it can be hard to realize the extent of the impairment. Noticing a consistent pattern of decline in these areas should serve as a strong signal to consult with a doctor or mental health professional.
The chronic nature of schizophrenia means it is a lifelong condition without a known cure in 2025. However, symptoms can be effectively managed with ongoing medication and therapy. Without proper management, symptoms can worsen over time, leading to significant distress and functional decline. While symptoms don’t always improve with age, consistent treatment can stabilize the condition. A significant challenge in reaching out for help is that individuals experiencing signs symptoms schizophrenia, especially paranoia or delusions, may feel suspicious of others, including healthcare providers. Reassurance and encouragement from trusted family members or friends can be instrumental in prompting someone to speak with a doctor or mental health professional, facilitating the crucial first step toward diagnosis and treatment (Harvard, 2024).