1. Understanding HPV: Types, Transmission, and Diagnosis
Human Papillomavirus (HPV) is not a single entity but a diverse group of over 150 related viruses, making it the most common sexually transmitted infection globally. Its prevalence means that the vast majority of sexually active individuals will be exposed to at least one type of HPV during their lifetime (CDC, 2024). Many people never even realize they have it, as their immune system often clears the infection without any symptoms appearing. However, some types can lead to noticeable physical manifestations or more serious health concerns.
The spectrum of HPV types ranges from low-risk variants that often cause genital warts to high-risk types that are responsible for cellular changes, which, if left untreated, can progress to various cancers, most notably cervical cancer. Other HPV-related cancers include those of the anus, vulva, vagina, penis, and oropharynx (back of the throat, including the base of the tongue and tonsils) (WHO, 2024). Transmission primarily occurs through skin-to-skin contact during sexual activity, including vaginal, anal, and oral sex. It’s crucial to understand that penetration is not required for transmission; intimate skin contact is sufficient. This fact often surprises individuals and highlights why condoms, while highly effective for many STIs, cannot completely prevent HPV transmission, as they don’t cover all exposed skin.
Diagnosing HPV itself can be complex because many types are asymptomatic. For individuals with a cervix, routine screening is paramount. The American Cancer Society recommends HPV testing for those aged 25 to 65, often performed concurrently with a Pap test (ACS, 2024). The HPV test specifically looks for high-risk types of the virus that are most likely to cause cancer, while the Pap test identifies abnormal cervical cells. If symptoms like genital warts appear, a healthcare provider can often diagnose them visually. For other types of HPV, there isn’t a routine screening test for men or for non-cervical areas, making awareness of symptoms and open communication with partners even more vital for living human papillomavirus responsibly.
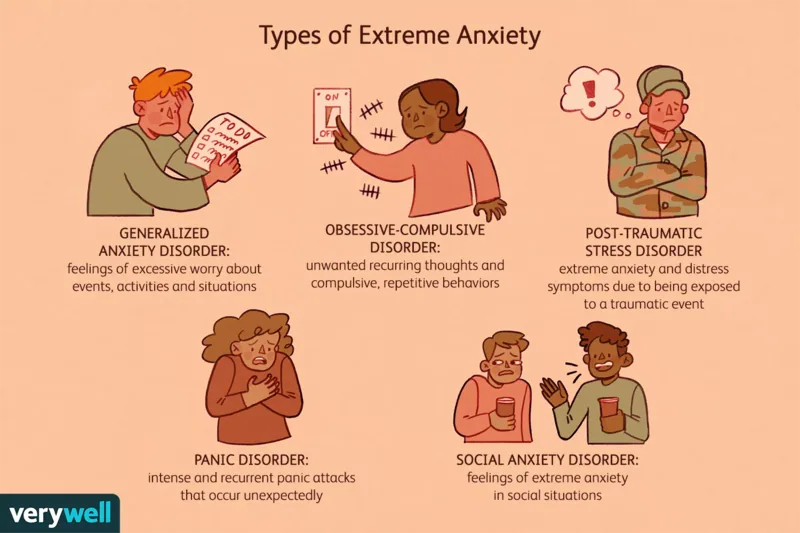
2. Navigating the Emotional Landscape of an HPV Diagnosis
Receiving an HPV diagnosis can be an emotionally challenging experience, often triggering a range of powerful feelings such as anxiety, shame, guilt, and even anger. Many individuals initially feel isolated or stigmatized due to misconceptions surrounding sexually transmitted infections. It’s common to worry about future health implications, potential impacts on relationships, and the overall perception of one’s sexual health. For instance, a common reaction is to question past relationships or feel a sense of betrayal, even though HPV can remain dormant for years, making it impossible to pinpoint the exact source or time of infection. This emotional burden can sometimes lead to withdrawal from social activities or a decrease in self-esteem, complicating the journey of living human papillomavirus.
However, it’s essential to reframe this initial shock with accurate information and self-compassion. HPV is incredibly common, and a diagnosis does not define your worth or your ability to lead a fulfilling life. Over time, many people learn to manage these emotions by seeking support and educating themselves further. For example, engaging with online forums or local support groups can provide a sense of community and shared experience, normalizing feelings that might initially feel overwhelming. Understanding that HPV often clears on its own and that proactive management can prevent serious health issues helps alleviate significant stress.
Seeking professional help, such as counseling or therapy, can also be immensely beneficial. Therapists specializing in sexual health or chronic conditions can provide strategies for coping with anxiety, depression, or body image concerns that may arise. They can help individuals process their feelings, challenge negative self-talk, and develop healthy communication skills for discussing their diagnosis with partners. Remember, an HPV diagnosis is a medical condition, not a moral failing. By actively addressing the emotional impact, individuals can regain a sense of control and confidence in their journey of living human papillomavirus.
3. Managing the Physical Realities and Health Implications
The physical manifestations and health implications of HPV vary widely depending on the specific strain of the virus involved. For many, HPV infections are asymptomatic and resolve without intervention. However, others may experience visible symptoms like genital warts, which are typically benign growths that can appear on the genitals, anus, or surrounding skin. While these warts can be bothersome or cause discomfort, they are treatable through various methods, including topical medications, cryotherapy (freezing), or surgical removal (Harvard, 2024). It’s important to note that treating warts does not eliminate the virus itself, but it manages the symptoms.
A more significant concern associated with high-risk HPV types is their potential to cause cellular changes that can lead to cancer. Cervical cancer is the most well-known, with nearly all cases linked to HPV (WHO, 2024). Thankfully, regular cervical cancer screenings, such as Pap tests and HPV tests, are highly effective in detecting these precancerous changes early. When caught early, these abnormal cells can be removed or treated, preventing cancer from developing. This proactive approach is a cornerstone of living human papillomavirus responsibly. Beyond cervical cancer, high-risk HPV can also contribute to cancers of the vulva, vagina, penis, anus, and oropharynx, emphasizing the importance of overall health monitoring.
Protecting yourself and others while living human papillomavirus involves several key strategies. Vaccination against HPV is a powerful preventive tool, recommended for adolescents before sexual activity, though it is approved for individuals up to age 26, and in some cases, up to 45 (CDC, 2024). For those already diagnosed, maintaining a robust immune system through a balanced diet, regular exercise, adequate sleep (at least eight to nine hours), and stress reduction is crucial. Some research suggests that chronic stress might hinder the immune system’s ability to clear HPV, potentially increasing cancer risk (Lugović-Mihić et al., 2021). Quitting smoking and reducing alcohol intake are also vital, as these habits can weaken immunity and exacerbate HPV-related risks.
4. Building a Supportive Social Network While Living with HPV
The social impact of an HPV diagnosis can be profound, often leading to feelings of isolation due to fear of judgment or misunderstanding from friends and family. The stigma associated with sexually transmitted infections can make it incredibly difficult for individuals to open up about their diagnosis, even to those closest to them. This silence, however, can exacerbate feelings of loneliness and prevent individuals from accessing the emotional support they need. It’s crucial to remember that HPV is extraordinarily common, and living human papillomavirus is a reality for millions, making shame an unnecessary burden.
Creating a robust support system begins with carefully choosing who to confide in. Selecting trusted friends or family members who are empathetic and open-minded can provide a safe space to discuss feelings and concerns. When sharing, it can be helpful to come prepared with accurate information to dispel common myths and alleviate any anxieties your loved ones might have. For example, explaining that HPV is not always indicative of infidelity, or that many infections clear on their own, can foster a more understanding environment. One individual, after her diagnosis, found immense relief in confiding in her older sister, who, to her surprise, shared that she too had experienced HPV years ago, instantly creating a bond of solidarity and understanding.
Beyond personal circles, connecting with formal support networks can be life-changing. Organizations like the National Cervical Cancer Coalition (NCCC) or the American Sexual Health Association (ASHA) offer resources, educational materials, and often facilitate support groups, both in-person and online. These groups provide a platform for individuals living human papillomavirus to share experiences, exchange coping strategies, and realize they are not alone. Engaging with these communities can counteract the stigma, transforming feelings of isolation into empowerment and connection, fostering resilience in the face of a challenging diagnosis.
5. Intimacy and Relationships: Open Communication with HPV
One of the most sensitive aspects of living human papillomavirus is navigating intimacy and relationships. The thought of disclosing an HPV diagnosis to a current or potential partner can be daunting, often triggering anxiety about rejection or misunderstanding. However, open, honest communication is the cornerstone of healthy sexual relationships, especially when an STI is involved. While it can be a difficult conversation, transparency allows both partners to make informed decisions about their sexual health and fosters trust.
When preparing to discuss your diagnosis, it’s helpful to educate yourself thoroughly about HPV so you can answer questions accurately and calmly. Explain that it’s very common, often asymptomatic, and that most people clear the virus naturally. Discuss the protective measures you can take, such as using condoms (which reduce but don’t eliminate risk) and regular screenings. For example, if you are in a committed relationship, your physician might advise discussing the diagnosis with your partner so they can speak with their own healthcare provider about screening or vaccination options, depending on their gender and age. This proactive approach ensures mutual responsibility for sexual health.
It’s also important to manage expectations and be prepared for a range of reactions. Some partners may be understanding and supportive, while others might need time to process the information or may react with fear or anger due to misinformation. A common misconception is that an HPV diagnosis indicates infidelity, which is often not the case given the virus’s long dormancy period. If your partner has been diagnosed with HPV, it’s crucial to approach the situation with empathy. Remember they likely had no intention of transmitting the virus and may not have even known they carried it. Prioritizing mutual respect, education, and shared decision-making strengthens the relationship, allowing intimacy to flourish even while living human papillomavirus.
6. Supporting Loved Ones: A Guide for Partners and Caregivers
When a partner, friend, or family member receives an HPV diagnosis, your support can make an immense difference in their emotional and physical well-being. It’s common for individuals with an STI to experience shame, guilt, or fear of stigma (Scheinfeld, 2021). Your role as a supporter is to counteract these feelings by offering unconditional empathy and reassurance. Start by reminding them that HPV is incredibly common, and their diagnosis is a medical condition, not a personal failing. Simply saying, “I’m here for you, and there’s nothing to be ashamed of,” can be incredibly powerful.
Educating yourself about HPV is another crucial step. Understanding the facts—that it’s widespread, often clears on its own, and can be managed—will equip you to provide informed support and dispel myths. This knowledge also helps you understand their potential health concerns, such as the importance of regular screenings or managing symptoms like genital warts. For instance, if your partner is navigating treatment for precancerous cells, you can offer to accompany them to appointments, help them track medication schedules, or simply be a comforting presence during what can be an anxious time. Your informed presence helps normalize their experience of living human papillomavirus.
Encourage open dialogue about their feelings and struggles. Create a safe space where they feel comfortable expressing their fears, anxieties, or frustrations without judgment. If they are considering joining a support group, offer to research options with them or even attend an initial meeting if appropriate. For partners, it’s also important to discuss your own sexual health with your healthcare provider to understand any potential implications for you, such as the need for HPV screening or vaccination. By being an active, informed, and compassionate ally, you can significantly ease the burden of living human papillomavirus for your loved one, fostering resilience and promoting their overall health.