Gabapentin, commonly recognized by its brand name Neurontin, is an anticonvulsant medication primarily prescribed to manage seizures and alleviate nerve pain. It’s also frequently used off-label for conditions like migraines, fibromyalgia, and various pain syndromes. If you’ve been taking gabapentin for an extended period, discontinuing its use can lead to a range of challenging symptoms. How long does withdrawal from gabapentin last? Typically, symptoms of withdrawal from gabapentin can manifest within 12 hours of the last dose and may persist for up to 7 days, though this timeline can vary significantly based on individual factors and dosage. It’s crucial to consult a healthcare provider before attempting to stop gabapentin to ensure a safe and managed process.
1. Understanding Gabapentin and Its Evolving Use
Gabapentin, marketed as Neurontin, is a medication classified as an anticonvulsant. Its primary indications include the management of partial seizures and the relief of neuropathic pain, such as postherpetic neuralgia. Beyond these approved uses, healthcare providers often prescribe gabapentin off-label to address conditions like restless legs syndrome, fibromyalgia, and certain types of migraines, highlighting its versatility in pain management and neurological disorders.
Despite its therapeutic benefits, the public perception and regulatory status of gabapentin have evolved considerably. While the U.S. Drug Enforcement Administration (DEA) has historically not classified gabapentin as a controlled substance due to a perceived low potential for abuse, several states have independently taken steps to do so. This shift reflects growing concerns surrounding its misuse.
The past decade has seen a significant increase in gabapentin prescriptions. As of 2025, current research indicates a continued rise in both prescribed use and, unfortunately, illicit abuse. This trend has led to an uptick in accidental overdose-related deaths, particularly when gabapentin is combined with other substances. This evolving landscape underscores the importance of understanding the risks associated with its use and discontinuation.
The widespread availability and increasing use of gabapentin mean that more individuals may encounter the challenges of withdrawal from gabapentin. This makes informed decision-making and professional medical guidance more critical than ever. Healthcare providers are continually updating their understanding of gabapentin’s effects and the best practices for its safe management.
2. Prevalence and Risk Factors for Gabapentin Withdrawal
While the experience of withdrawal from gabapentin is often described as rare, the current understanding suggests it may be more common than previously documented. Early medical journal reviews, spanning from gabapentin’s approval in 1993 to 2015, identified only a handful of case reports detailing addiction, dependence, or withdrawal. These reports, often published by healthcare providers encountering unusual patient conditions, play a vital role in expanding medical knowledge and identifying areas for further research.
The low number of reported cases does not necessarily equate to true rarity. Many individuals experiencing milder symptoms of gabapentin withdrawal might not seek professional medical attention, leading to an underestimation of its true prevalence. Experts anticipate that as gabapentin use continues to climb, more cases of withdrawal will likely emerge. The DEA noted a doubling of gabapentin prescriptions between 2011 and 2021, reaching over 70 million prescriptions in the latter year, indicating a larger population potentially at risk.
A significant risk factor for experiencing withdrawal from gabapentin appears to be the concurrent use of other substances, particularly opioids or alcohol. Case reports frequently show that patients experiencing gabapentin dependence or withdrawal often have a history of polysubstance abuse. For instance, some opioid users have reported using gabapentin to intensify their high, while cocaine users have used it in attempts to alleviate their own withdrawal symptoms.
Consider a scenario where a person struggling with opioid use might start using gabapentin to try and ‘soften’ opioid withdrawal symptoms, inadvertently developing a dependence on gabapentin as well (Harvard, 2024). This highlights how gabapentin can become entangled in complex substance use patterns, increasing the likelihood of experiencing severe withdrawal symptoms when discontinued. This interaction with other drugs underscores the need for comprehensive screening and treatment for individuals at risk.
3. The Gabapentin Withdrawal Timeline
Understanding the timeline for withdrawal from gabapentin is crucial for anyone considering discontinuing the medication. Based on documented cases, the onset of withdrawal symptoms can occur relatively quickly, typically beginning anywhere from 12 hours to 7 days after the last dose. For the majority of individuals, symptoms tend to emerge within 24 to 48 hours, aligning with the drug’s half-life and how quickly it is cleared from the body.
Once symptoms begin, they generally follow a predictable pattern. The peak intensity of gabapentin withdrawal symptoms is most commonly observed around three days after the final dose. This period is often the most challenging, characterized by heightened discomfort and a greater risk of severe reactions. The overall duration of acute withdrawal can last up to 7 days in many reported instances.
However, it’s important to recognize that the timeline can vary significantly. Factors such as the dosage of gabapentin taken, the duration of its use, and individual metabolic rates can all influence how quickly and intensely symptoms develop and resolve. Higher doses and longer periods of use are generally associated with more severe and prolonged withdrawal experiences.
In almost all documented cases where severe symptoms of withdrawal from gabapentin were reported, healthcare providers effectively managed them by temporarily resuming the patient’s previous gabapentin dose. Once the medication was reintroduced, symptoms typically subsided within hours. This immediate response underscores the drug-specific nature of the withdrawal and the effectiveness of re-stabilization. Imagine Sarah, who typically takes her gabapentin every evening. One weekend, she travels and forgets her medication. By Sunday afternoon (around 36 hours later), she starts feeling unusually agitated and experiences tremors, realizing it’s due to the sudden stop. This illustrates a common, unexpected onset of symptoms.
4. Recognizing Symptoms of Gabapentin Withdrawal
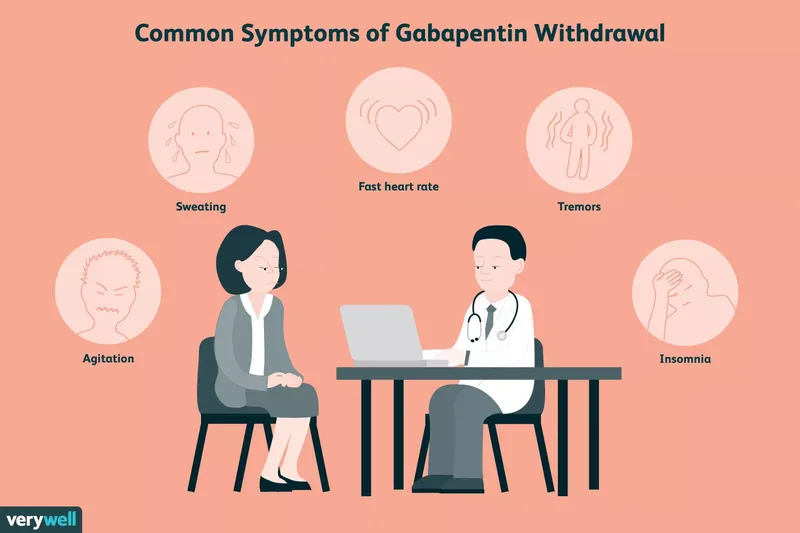
Recognizing the signs and symptoms of withdrawal from gabapentin is essential for timely intervention and safe management. The most frequently reported symptom is agitation, affecting approximately half of the individuals who experience withdrawal. This agitation can range from restlessness to severe anxiety and irritability, making daily functioning challenging.
Following agitation, confusion and disorientation are common, often leading to a sense of unreality or difficulty processing thoughts. Other notable symptoms include increased sweating, which can be profuse and uncomfortable, and various gastrointestinal issues such as nausea, vomiting, or diarrhea. Physical manifestations often include tremors, which are involuntary muscle quivering, and physiological changes like a fast heart rate (tachycardia) and elevated blood pressure (hypertension). Insomnia is also a prominent symptom, severely disrupting sleep patterns and exacerbating other discomforts.
What are the common symptoms of gabapentin withdrawal? Common symptoms include agitation, confusion, sweating, gastrointestinal upset, tremors, fast heart rate, high blood pressure, and insomnia. These can emerge within hours of stopping the medication.
It’s important to note that many individuals documented in medical journals entered gabapentin withdrawal unintentionally. This often occurred due to running out of their medication unexpectedly or forgetting it while traveling. These unplanned interruptions highlight how easily withdrawal can be triggered in dependent individuals, even without a deliberate attempt to stop.
This sample of reported cases, however, may not fully represent the spectrum of experiences with withdrawal from gabapentin. People are more likely to seek emergency medical treatment for severe or alarming symptoms, meaning milder cases might go unreported. Therefore, while these documented symptoms are critical to be aware of, the full range of experiences could be broader and less dramatic for some individuals.
5. Professional Treatment for Gabapentin Discontinuation
There are currently no standardized clinical protocols specifically designed to manage withdrawal from gabapentin. Therefore, a personalized approach developed in close collaboration with your healthcare provider is essential. This plan will consider your pre-existing medical conditions, any history of substance abuse, and the original reasons you were prescribed gabapentin.
The general medical consensus strongly advocates for tapering off the medication rather than stopping abruptly. Tapering involves gradually reducing your dose over a period of time, which significantly helps to prevent the onset of severe gabapentin withdrawal symptoms. While some individuals might attempt to taper at home, maintaining open and regular communication with your doctor is paramount to ensure safety and effectiveness.
If you have been taking high doses of gabapentin under a doctor’s prescription, it is absolutely critical to consult that doctor before initiating any tapering process or discontinuing the medication on your own. Your healthcare provider will meticulously discuss the potential risks and benefits of stopping gabapentin, which can include the return of seizures, exacerbation of opioid dependence if that was a co-occurring issue, or a resurgence of your original pain condition.
What is the best way to stop gabapentin? The safest and most recommended way to stop gabapentin is through a gradual tapering process, designed and supervised by your healthcare provider, to minimize severe withdrawal symptoms.
Depending on your specific situation, your doctor might recommend transitioning to an alternative medication before completely tapering off gabapentin. This strategy can help manage underlying conditions and ease the transition. For instance, a doctor might prescribe a different nerve pain medication before slowly reducing gabapentin, ensuring continuous symptom management (Harvard, 2024).
For individuals who have been abusing their gabapentin prescription, particularly by mixing it with other drugs or alcohol, tapering alone may not be sufficient. Addiction is a complex neurological disorder that necessitates a comprehensive, long-term treatment plan. Such programs typically integrate various therapeutic approaches to address the root causes of substance abuse, provide coping mechanisms, and support sustained recovery.
6. Coping Strategies for Managing Withdrawal Symptoms
Coping effectively with withdrawal from gabapentin symptoms hinges on several factors, including the severity of your symptoms, your overall mental and physical health, your current gabapentin dosage, and your reasons for taking the medication. The overarching principle is to prioritize safety and seek medical guidance.
If you or a loved one are already experiencing significant gabapentin withdrawal symptoms, especially severe confusion or psychosis, immediate medical attention is warranted. In these acute situations, taking the individual to an emergency room is crucial. Paradoxically, the most effective immediate treatment for severe gabapentin withdrawal symptoms, such as delirium, is often the reintroduction of gabapentin at a normal dose. This can rapidly alleviate dangerous symptoms and stabilize the individual.
After stabilizing on your normal dose, the next step is to schedule an appointment with your healthcare provider. This consultation will allow you to discuss your motivations for discontinuing gabapentin and develop a safe, medically supervised tapering plan. Tapering involves progressively smaller doses of the medication over an extended period, which can range from several weeks to months, and in some complex cases, even over a year.
How slowly should you come off gabapentin? The pace of tapering off gabapentin varies greatly, depending on your prescribed dosage, duration of use, and any co-existing health conditions; it can take weeks, months, or even over a year under medical supervision.
John, prescribed gabapentin for nerve pain, decides with his doctor to slowly reduce his dose. Over several months, he gradually decreases his daily intake, monitoring for any returning pain or mild anxiety. His doctor provides a schedule and checks in weekly to adjust as needed, allowing him to manage the transition smoothly at home. During this time, supportive care such as maintaining good hydration, ensuring adequate rest, and engaging in light, stress-reducing activities can also aid in managing milder symptoms. Psychological support, like therapy or counseling, can also be invaluable for addressing any underlying anxieties or mental health challenges that may arise during the withdrawal process.
7. Important Warnings and Special Considerations
While the understanding of withdrawal from gabapentin is still evolving, the documented cases present alarming insights, particularly for individuals with specific risk factors. Many of the reported case studies involve people with a history of psychiatric disorders or substance abuse problems. If you fall into either of these categories, there is heightened cause for concern and a need for extreme caution when considering gabapentin discontinuation.
Pre-existing Conditions: A critical warning is the potential for pre-existing conditions to resurface or worsen during detox and gabapentin withdrawal. Individuals with a history of bipolar disorder, psychosis, depression, or epilepsy are particularly vulnerable. The withdrawal process can trigger a return of symptoms to pretreatment levels, or even exacerbate them. Similarly, if gabapentin was prescribed for pain management, that pain is likely to return, potentially with increased intensity. For these high-risk individuals, undergoing detox in a hospital setting or a specialized inpatient facility is often the safest option. Healthcare providers in such environments are equipped to monitor for and treat any potential complications, ensuring a more secure withdrawal process.
Pregnancy: Gabapentin use during pregnancy also presents unique considerations and potential risks. There is a documented case study where an infant was admitted to the neonatal intensive care unit (NICU) because she was born experiencing gabapentin withdrawal symptoms. This highlights the possibility of neonatal withdrawal syndrome, where the baby experiences withdrawal from exposure to the drug in utero. If you are pregnant and taking gabapentin, it is imperative to have a thorough discussion with your obstetrician. They can assess the safety of continuing gabapentin during pregnancy and help you explore the possibility of a safe tapering plan before your baby is born, mitigating potential risks to the newborn.
These warnings underscore that discontinuing gabapentin, especially in the presence of complicating factors, is a serious medical undertaking that should never be attempted without professional guidance.
8. Finding Support and Resources
Navigating withdrawal from gabapentin requires a strong support system and access to appropriate resources. If you or someone you care about experiences serious symptoms of gabapentin withdrawal, such as profound confusion, disorientation, or delirium, do not hesitate to seek emergency medical attention immediately. These symptoms can be dangerous and require urgent professional intervention.
For those planning to stop taking gabapentin, the first crucial step is to make an appointment with your prescribing physician or a primary care doctor. These professionals are best equipped to guide you through a safe tapering process, monitor your progress, and adjust your plan as needed. They can also provide referrals for additional support if necessary.
If you are struggling with broader addiction issues, particularly if you have been combining gabapentin with other drugs or alcohol, finding long-term support is essential for sustainable recovery. Fortunately, several options are available:
- Mental Health Professionals: A psychologist, psychiatrist, or counselor, whether in private practice or affiliated with a hospital, can offer individual therapy, group sessions, and medication management for co-occurring mental health conditions.
- Inpatient Detox Facilities: These specialized centers provide a medically supervised environment for safe detoxification, particularly beneficial for individuals at high risk of severe withdrawal symptoms or with complex substance use histories.
- Addiction Treatment Centers: Many centers offer comprehensive inpatient or outpatient programs that combine therapy, counseling, and peer support to address the underlying causes of addiction and develop coping strategies.
- Peer Support Groups: Organizations like Narcotics Anonymous (NA) provide a supportive community where individuals can share experiences and work through a structured program of recovery (Harvard, 2024).
- Medication-Assisted Treatment (MAT) Providers: For those with opioid dependence, a provider licensed to distribute buprenorphine can offer crucial support as part of an overall treatment plan.
If you or a loved one are struggling with substance use or addiction, please contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357. This confidential helpline can provide information on support and treatment facilities available in your local area.
Conclusion
Understanding withdrawal from gabapentin is crucial for anyone prescribed this medication, especially given its increasing prevalence and evolving misuse concerns. While often considered rare, the potential for dependence and significant withdrawal symptoms is real, particularly for those with a history of substance abuse or psychiatric conditions. Symptoms can range from agitation and confusion to physical manifestations like tremors and high blood pressure, typically emerging within 12 hours to 7 days after the last dose and peaking around three days.
It is paramount to emphasize that abruptly stopping gabapentin is dangerous and should never be attempted without medical supervision. A carefully managed, gradual tapering plan, developed in consultation with your healthcare provider, is the safest and most effective strategy to minimize discomfort and prevent severe complications. For those with co-occurring addiction issues, a comprehensive, long-term treatment plan is essential for lasting recovery. Seeking professional guidance and utilizing available support resources are critical steps toward a safe and successful discontinuation of gabapentin.