Navigating mental health treatment can feel overwhelming, especially when considering new medications. Lexapro, known generically as escitalopram, is a widely prescribed antidepressant that can significantly improve symptoms of depression and anxiety. However, understanding its full scope—from how it works to potential side effects and interactions—is crucial before taking Lexapro. This comprehensive guide outlines everything you need to know about Lexapro in 2025, empowering you to make an informed decision with your healthcare provider.
Core Insight: Lexapro is an effective SSRI that helps balance brain chemistry to alleviate mood and anxiety disorders, but requires careful consideration of individual health, potential side effects, and adherence to medical guidance for safe and effective use.
Key Points to Consider Before Taking Lexapro:
- Mechanism of Action: Lexapro works by increasing serotonin levels in the brain, a key neurotransmitter for mood regulation.
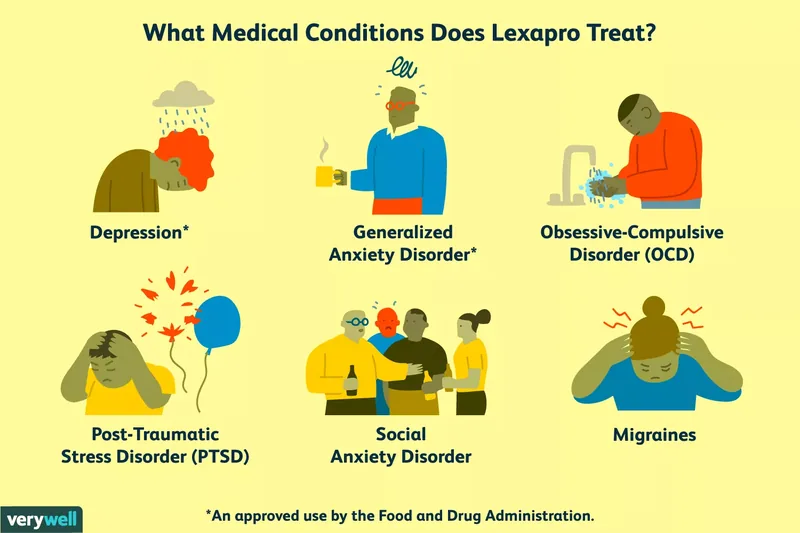
- Diverse Applications: While primarily for depression and GAD, it’s also prescribed off-label for conditions like OCD and PTSD.
- Crucial Precautions: Discuss your full medical history, current medications, and any allergies with your doctor to avoid adverse effects.
- Managing Expectations: Full therapeutic benefits can take several weeks, and side effects often diminish over time.
- Safe Discontinuation: Never stop Lexapro abruptly; always taper off under professional medical supervision to prevent withdrawal symptoms.
Deciding to start an antidepressant like Lexapro is a significant step towards better mental well-being. This guide will help you understand the essential aspects of this medication, ensuring you are fully prepared before taking Lexapro.
1. Understanding Lexapro: Uses and Efficacy
Lexapro, the brand name for escitalopram, is a selective serotonin reuptake inhibitor (SSRI) commonly prescribed for various mental health conditions. Introduced following its predecessor citalopram, escitalopram is known for its effectiveness in treating major depressive disorder (MDD) and generalized anxiety disorder (GAD). For individuals struggling with persistent sadness, loss of interest, or excessive worry, Lexapro offers a pathway to symptom relief and improved quality of life. Its role as an SSRI means it works on specific neurotransmitters, making it a targeted treatment option compared to older classes of antidepressants (Santarsieri & Schwartz, 2015).
Beyond its primary indications, healthcare providers may also prescribe Lexapro off-label for other conditions where it has shown benefit. These can include obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), social anxiety disorder, and even premenstrual dysphoric disorder (PMDD) (U.S. National Library of Medicine, 2024). The decision to use Lexapro for these conditions is typically based on a doctor’s clinical judgment and the patient’s specific symptoms and response to treatment. For example, a patient with severe social anxiety impacting their daily life might find Lexapro helpful in reducing their fear of social situations, allowing them to engage more freely. Similarly, someone with intrusive thoughts and compulsive behaviors from OCD might experience a significant reduction in symptom severity.
It’s important to remember that Lexapro is not a one-size-fits-all solution. If it doesn’t provide the desired relief, your doctor will work with you to explore alternative treatments. This could involve trying a different SSRI, an antidepressant from another class (such as an SNRI), or integrating psychotherapy. Often, a combination of medication and therapy yields the most robust and lasting results for many individuals (Harvard, 2024). Understanding these diverse applications and the potential for individualized treatment plans is an important step before taking Lexapro.
2. How Lexapro Works to Improve Mood
The precise mechanisms by which antidepressants like Lexapro exert their full effects are still subjects of ongoing research. However, the prevailing understanding centers on its action as a selective serotonin reuptake inhibitor (SSRI). Serotonin is a crucial neurotransmitter, a chemical messenger in the brain that plays a significant role in regulating mood, sleep, appetite, and various other functions. In individuals with depression or anxiety, serotonin levels in the brain’s synaptic cleft (the space between neurons) may be imbalanced or too low.
Lexapro works by binding to the serotonin transporter protein (SERT) on the presynaptic neuron. Normally, SERT is responsible for “reuptaking” or reabsorbing serotonin from the synaptic cleft back into the presynaptic neuron, effectively reducing the amount of serotonin available to other neurons. By inhibiting this reuptake process, escitalopram leads to an elevation in serotonin levels within the synaptic cleft (Landy et al., 2024). This increased availability of serotonin allows it to bind more readily to receptors on the postsynaptic neurons, enhancing serotonin signaling.
This enhanced serotonin signaling is thought to contribute to the mood-boosting and anxiety-reducing effects of Lexapro. It’s not an immediate process; the brain needs time to adapt to these altered serotonin levels, which is why it can take several weeks to experience the full therapeutic benefits. The brain’s complex neurochemistry involves many interconnected systems, and Lexapro’s influence on serotonin can have downstream effects on other neurotransmitter systems and neural circuits (Harvard, 2024). This gradual adjustment period highlights the importance of consistent medication use as prescribed by your doctor. Understanding this fundamental mechanism provides valuable insight into what happens in your body before taking Lexapro and throughout your treatment journey.
3. Important Considerations Before Taking Lexapro
Prior to starting Lexapro, a thorough discussion with your healthcare provider is paramount to ensure it’s the right and safest option for you. Generally, Lexapro is prescribed following a mental health diagnosis such as generalized anxiety disorder or major depressive disorder. While a primary care physician can prescribe it, consulting with a mental health professional like a psychiatrist or psychiatric nurse practitioner can offer a more comprehensive treatment approach, often combining medication with psychotherapy (National Alliance on Mental Illness, 2024). This holistic view is critical before taking Lexapro.
It is absolutely essential to disclose your complete medical history to your doctor. This includes any known allergies or hypersensitivities to escitalopram or similar medications. Furthermore, inform them if you are pregnant, planning to become pregnant, or breastfeeding, as Lexapro can pass to the child and may carry risks, particularly if taken later in pregnancy (FDA, 2024). Your doctor needs to be aware of any pre-existing medical conditions that could be exacerbated by Lexapro, such as:
- Bipolar disorder: SSRIs can sometimes trigger manic or hypomanic episodes in individuals with undiagnosed bipolar disorder.
- Glaucoma: Lexapro may increase intraocular pressure in some cases.
- Low sodium levels (hyponatremia): Older adults are particularly susceptible to this side effect.
- Seizure disorders: Lexapro can lower the seizure threshold.
- History of suicidal thoughts or behaviors: Close monitoring is crucial, especially in younger individuals, due to the black box warning.
Additionally, provide a comprehensive list of all medications, supplements, and vitamins you are currently taking. This includes over-the-counter drugs, herbal remedies like St. John’s wort, and even recreational substances. Certain combinations can lead to dangerous interactions, such as serotonin syndrome, or increase the risk of bleeding. A detailed pre-Lexapro checklist with your doctor helps mitigate these risks and ensures your safety and well-being. This comprehensive pre-assessment is a non-negotiable step before taking Lexapro.
4. Lexapro Dosage and Administration Guidelines
Understanding the correct dosage and how to administer Lexapro is crucial for its effectiveness and safety. Lexapro is available in tablet form, typically in 5 mg, 10 mg, and 20 mg strengths, with the 10 mg and 20 mg tablets often scored for easier halving. An oral solution, 1 mg per milliliter (mL), is also available for those who have difficulty swallowing pills. The standard starting dose for adults with major depressive disorder or generalized anxiety disorder is usually 10 mg once daily. However, your doctor might initiate treatment at a lower dose, such as 5 mg, and gradually increase it to 10 mg after a week, based on your tolerance and response.
For adolescents aged 12 to 18 with major depressive disorder, the recommended starting dose is also 10 mg per day, with the option to increase to 20 mg after three weeks if clinically necessary. It’s important to note that dosages higher than 20 mg are not approved by the FDA, as increasing the dose beyond this point typically does not confer additional benefits but can heighten the risk of side effects. Dosage adjustments may also be necessary for specific populations, such as older adults or individuals with severe kidney impairment, who may require a lower starting dose and careful monitoring due to altered drug metabolism (Ortiz, 2020).
Lexapro can be taken once daily, either in the morning or evening, with or without food, depending on what best suits your routine and minimizes potential side effects like drowsiness or insomnia. Consistency is key, so try to take it at roughly the same time each day. If a dose is missed, take it as soon as you remember, unless it’s almost time for your next scheduled dose, in which case you should skip the missed dose and resume your regular schedule. Never double up on doses. It’s vital to manage expectations regarding the onset of action; while some improvements in sleep or energy may be noted within the first week or two, the full antidepressant or anxiolytic effects can take anywhere from one to two months to manifest (National Alliance on Mental Illness, 2024). Patience and adherence to your prescribed regimen are essential before taking Lexapro and throughout your treatment.
5. Potential Side Effects of Lexapro
Like all medications, Lexapro can cause side effects, although many people tolerate it well, and most common side effects tend to diminish as your body adjusts. It’s important to discuss any concerns with your doctor before taking Lexapro and throughout your treatment. The most frequently reported side effects of escitalopram often include gastrointestinal issues, neurological symptoms, and changes in sleep patterns. Common side effects may include nausea, headaches, dry mouth, and sleep disturbances such as insomnia or drowsiness. Other potential effects are diarrhea or constipation, stomach pain, heartburn, lightheadedness, dizziness, and increased sweating. Some individuals may also experience irritability, nervousness, fatigue, or flu-like symptoms. Sexual side effects, such as decreased libido or difficulty achieving orgasm, are also common with SSRIs (U.S. National Library of Medicine, 2024).
While these common side effects are typically mild and transient, it’s crucial to monitor them. If they persist, worsen, or significantly impact your quality of life, contact your healthcare provider. For example, if initial nausea is severe, your doctor might suggest taking the medication with food or adjusting the time of day you take it. Persistent sleep issues might lead to a discussion about taking it in the morning versus evening. Open communication with your doctor allows for adjustments that can improve your experience.
In rare instances, Lexapro can cause more severe side effects that require immediate medical attention. These include difficulty breathing or swallowing, swelling of the face, mouth, or tongue (signs of an allergic reaction), fever, stiff muscles, fast heartbeat, seizures, rash, confusion, or hallucinations. A serious but rare condition known as serotonin syndrome can occur, especially if Lexapro is taken with other serotonergic drugs. Symptoms of serotonin syndrome include agitation, hallucinations, rapid heartbeat, fever, overactive reflexes, nausea, vomiting, diarrhea, and uncoordinated movements (Kulkarni & Kulkarni, 2013). If you experience any of these severe symptoms, seek emergency medical care without delay. Being aware of these potential reactions is a critical part of your knowledge before taking Lexapro.
6. Warnings, Interactions, and Discontinuation of Lexapro
Lexapro carries important warnings and can interact with numerous other medications, making a full disclosure of your medical history and current drug regimen imperative before taking Lexapro. The most serious warning is a “black box warning” issued by the FDA concerning an increased risk of suicidal thoughts and behaviors, particularly in children, adolescents, and young adults. Close monitoring by a psychiatrist or doctor is essential, especially during the initial weeks of treatment or whenever the dosage is adjusted. If you or a loved one experience suicidal thoughts, immediately contact emergency services or a crisis hotline like 988.
Several medications should be avoided or used with extreme caution due to the heightened risk of serotonin syndrome when combined with Lexapro. These include other SSRIs, tricyclic antidepressants (TCAs), triptans (used for migraines), and most critically, monoamine oxidase inhibitors (MAOIs). You should not take MAOIs within 14 days of starting or stopping escitalopram (University of Michigan Health, 2024). Other drugs that can negatively interact include blood thinners like warfarin, aspirin, and NSAIDs, which can increase the risk of bleeding. The antibiotic linezolid is another significant concern, as its combination with escitalopram has been linked to life-threatening serotonin syndrome (Kulkarni & Kulkarni, 2013). Always inform your doctor about all prescription and over-the-counter medications, herbal supplements (like St. John’s wort), and recreational drugs you use. Additionally, avoid alcohol while on Lexapro, as it can worsen side effects and reduce the medication’s effectiveness.
Discontinuing Lexapro should always be done under the careful guidance of a healthcare professional. Abruptly stopping the medication can lead to withdrawal symptoms, often referred to as antidepressant discontinuation syndrome. These symptoms can include dizziness, muscle tension, chills, confusion, trouble concentrating, memory issues, and crying spells (Yasui-Furukori et al., 2016). Your doctor will typically create a tapering schedule, gradually reducing your dose over several weeks or months to minimize these effects. This slow reduction allows your brain to adjust to the decreasing serotonin levels. For instance, if you are switching to another SSRI, your doctor might recommend a gradual reduction of Lexapro over a four-week period while slowly introducing the new medication. Never attempt to stop Lexapro on your own; always consult your doctor to ensure a safe and managed discontinuation process. This careful approach to stopping is as critical as what to know before taking Lexapro.
Frequently Asked Questions
When is the best time to take Lexapro for anxiety? The optimal time to take Lexapro for anxiety often depends on how your body reacts to the medication. If Lexapro tends to make you drowsy, taking it in the evening might be beneficial for sleep. Conversely, if it makes you feel more alert or causes insomnia, a morning dose could be more appropriate. Discussing your specific side effects with your doctor will help determine the best time for your individual needs.
How does Lexapro make you feel the first week? During the first week of taking Lexapro, you are unlikely to experience significant improvements in your depression or anxiety symptoms. Instead, you might notice some common side effects such as headaches, nausea, diarrhea, dry mouth, nervousness, restlessness, fatigue, insomnia, or increased sweating. These initial side effects usually subside within one to two weeks as your body adjusts to the medication.
How long does it take Lexapro to work? While some initial improvements, like better sleep, increased energy, or a normalized appetite, might be observed within the first couple of weeks of taking Lexapro, the full therapeutic benefits often take longer. It can typically take anywhere from four to eight weeks, or even longer for some individuals, to experience the complete antidepressant and anxiolytic effects of the medication. Consistent adherence to your prescribed regimen is key.
What should you expect when increasing Lexapro dosage? When your doctor increases your Lexapro dosage, you may temporarily experience side effects similar to those you felt when first starting the medication, possibly for a day or two. Your doctor will likely want to monitor you closely during this period to ensure your condition doesn’t worsen and that you don’t develop any significant negative side effects. Open communication about any changes you observe is vital.
Why does Lexapro cause weight gain? Lexapro can lead to weight gain for several reasons. It impacts serotonin levels, which are known to influence appetite and metabolism. Some research suggests that individuals with a lower body mass index before starting Lexapro, those with lower educational status, or those with a family history of obesity might be at a higher risk of experiencing weight gain while on this medication (Uguz et al., 2015). Discussing dietary and lifestyle strategies with your doctor can help manage this.
How do you know if Lexapro is working? Lexapro’s effects are typically gradual rather than sudden. You can assess its effectiveness by regularly reflecting on your mood, anxiety levels, energy, and overall well-being compared to before starting the medication. Keeping a journal or using a mood tracking app can help you identify subtle improvements over time. If after several weeks you notice no change or a worsening of symptoms, contact your doctor to discuss potential adjustments.
What happens if you overdose on Lexapro? An overdose of Lexapro can be serious and requires immediate medical attention. One notable effect of a Lexapro overdose is the potential for heart rhythm issues, specifically an extended QT interval, which refers to prolonged intervals between heart contractions and relaxations (Howland, 2012). Symptoms can also include dizziness, tremor, agitation, confusion, and seizures. If you suspect an overdose, call 911 or your local emergency number immediately.
Keep in Mind
This comprehensive guide offers essential information about Lexapro, covering its uses, mechanisms, precautions, dosage, side effects, and interactions. However, it is not a substitute for professional medical advice. Always consult with a qualified healthcare provider to discuss your specific health needs and any questions you have before taking Lexapro. Your doctor can provide personalized guidance and ensure the safest and most effective treatment plan for you.