Therapy
Looking Deeper at Veterans: The Complete 2025 Guide
On Veterans Day—and every day—it’s not enough to say "thank you" and move on. The real act of honor is looking deeper at veterans’ lives, especially the invisible wounds that follow them home.
In the first 100 words, here’s the answer many people search for: The most meaningful way to support veterans is to recognize their unique mental health challenges, avoid intrusive questions, use informed language, and connect them with evidence-based care and community support designed specifically for their experiences.
Why Looking Deeper at Veterans Matters
Behind every uniform is a complex story of transition, trauma, loyalty, loss, resilience—and often, quiet struggle.
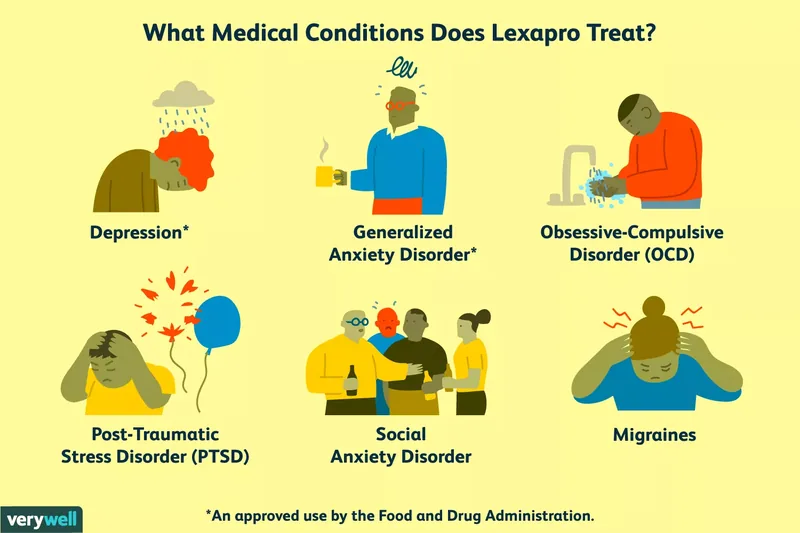
Data from the VA and leading researchers shows elevated rates of PTSD, depression, traumatic brain injury, and substance use disorders among veterans compared to civilians.
Stanford researchers and experts at Harvard (2024) emphasize that early, culturally informed intervention dramatically improves outcomes.
The call in 2025 is clear: We must move beyond symbolic gestures and step into informed, compassionate action.
People Also Ask: What Do Veterans Really Need on Veterans Day?
A powerful starting point is simple:
- Offer sincere appreciation without demanding personal details.
- Listen without judgment if they choose to share.
- Support access to specialized mental health and addiction care.
A respectful approach helps veterans feel seen as whole people—not headlines, not stereotypes, and not a single chapter of their service record.
Key Insight: The Invisible Load Many Veterans Carry
Looking deeper at veterans means acknowledging that the end of deployment is rarely the end of impact.
Many post‑9/11 veterans screen positive for at least one mental health condition, and a significant portion report difficulties with sleep, hypervigilance, moral injury, and reintegration.
Short, critical realities:
- Veterans face heightened risk for suicidal thoughts and behaviors.
- Over 1 in 10 lives with a substance use disorder, with alcohol most common.
- PTSD, TBI, chronic pain, and family strain often interact, not exist in isolation.
In everyday life, this can look like irritability at crowded events, avoiding fireworks, overworking, withdrawing from social circles, or joking about experiences that feel "too dark" for others to understand.
How to Honor Veterans Without Doing Harm
If you’re committed to looking deeper at veterans, shift from curiosity to care.
Here are grounded, respectful ways to show support:
- Start with: "Thank you for your service" — and then follow their lead.
- Avoid: "Did you kill anyone?" "Did you see combat?" or "How bad was it?".
-
Use open-ended, non-intrusive questions, such as:
- "What did your service teach you about leadership or teamwork?"
- "Is there anything about military life you wish more civilians understood?"
- Respect silence. Not every veteran wants, needs, or benefits from revisiting trauma.
- Learn the basics of military culture and terminology so conversations feel less clumsy and more respectful.
Three everyday examples:
- At work, instead of spotlighting someone in a meeting without asking, quietly check in and ask if/how they’d like their service acknowledged.
- If your gym has many veterans, advocate for a clear notice before any loud simulated gunfire or explosive sound effects during events.
- When a friend who served turns down a busy bar or fireworks show, don’t push—offer an alternative that feels safer.
These small choices send a clear message: "You don’t have to perform your story for my comfort."
People Also Ask: What Mental Health Support Works Best for Veterans?
For many veterans, generic "talk therapy" isn’t enough.
They benefit most from evidence-based, culturally competent care tailored to the realities of service.
Effective approaches include:
- Cognitive Behavioral Therapy (CBT): To challenge beliefs shaped by trauma and operational stress.
- Acceptance and Commitment Therapy (ACT): To help veterans live by their values while carrying painful memories.
- EMDR and trauma-focused therapies: To process combat trauma, moral injury, and life-threatening events.
- Seeking Safety and integrated care: For co-occurring PTSD and substance use.
- Post-traumatic growth frameworks: To explore meaning, identity, and strength after trauma.
Harvard (2024) experts underscore that when these treatments are paired with strong social support and veteran-informed care environments, outcomes significantly improve.
A Quick Guide for Therapists Working With Veterans
If you’re a clinician, looking deeper at veterans is a professional responsibility, not an optional niche.
Key principles:
- Build veteran cultural competence: Learn ranks, branches, deployment cycles, unit cohesion, and the concept of "moral injury".
- Collaborate with local VA and community veteran programs to ensure continuity of care.
- Whenever possible, offer veteran-only or first responder groups for combat-related trauma.
-
Design your office thoughtfully:
- Neutral, respectful decor (avoid glamorizing combat or heavy partisan messaging).
- Clear privacy, predictable scheduling, minimized chaotic noise.
-
Stay grounded when hearing "war stories"—avoid sensational reactions.
Your calm signals safety. - Ask directly: "What would help you feel respected and understood in this space?"
Bold reminder: Veterans are experts on their own experience. Co-create treatment, don’t impose it.
People Also Ask: How Can Friends and Families Support Without Overstepping?
Support doesn’t require clinical training. It does require consistency, humility, and willingness to see beyond stereotypes.
Try this simple framework:
- Be present: Check in with a short text or call on ordinary days, not just holidays.
- Use clear, nonjudgmental language about mental health and substance use.
- Normalize help: "Talking to someone is a strength move, not a failure."
-
Offer practical support:
- Help with appointments or transportation.
- Share vetted resources for veteran-specific services.
- Create routines—walks, workouts, coffee—that give structure and connection.
Looking deeper at veterans in your life means asking, "What does support look like for you right now?"—and then listening to the answer.
One Action Step You Can Take Today
Choose one veteran in your world—family member, colleague, neighbor, teammate.
Today, send a short, genuine message:
"Thinking of you and your service today. No pressure to share anything, but if there’s ever a way I can support you—mentally, practically, or just by listening—I’m here."
This small act can open a door far more meaningful than a one-day thank you.
If You or a Veteran You Love Is in Crisis
If you or someone you care about is contemplating suicide or feeling unsafe, seek help immediately.
- Call or text 988 in the U.S. for the Suicide & Crisis Lifeline (24/7).
- In an emergency, contact local emergency services or go to the nearest ER.
- For ongoing support, connect with a licensed mental health professional who understands veteran experiences.
Looking deeper at veterans means not waiting until "it’s really bad" to reach out. The earlier we support, the more lives—and futures—we protect.