Proven Breakthrough: Ketamine Found Effective for Chronic Pain Relief
Chronic pain profoundly impacts millions, often leaving individuals searching for effective relief when standard treatments fail. A significant new study offers a beacon of hope, revealing that low-dose ketamine infusions can be both safe and remarkably effective for patients battling chronic refractory pain. This breakthrough suggests that ketamine, traditionally known as an anesthetic, could become a crucial therapeutic tool, particularly for those whose severe, persistent pain has resisted conventional interventions. The findings are a pivotal step towards wider acceptance and potential FDA approval, providing a new pathway to improved quality of life for many suffering individuals.
Key points
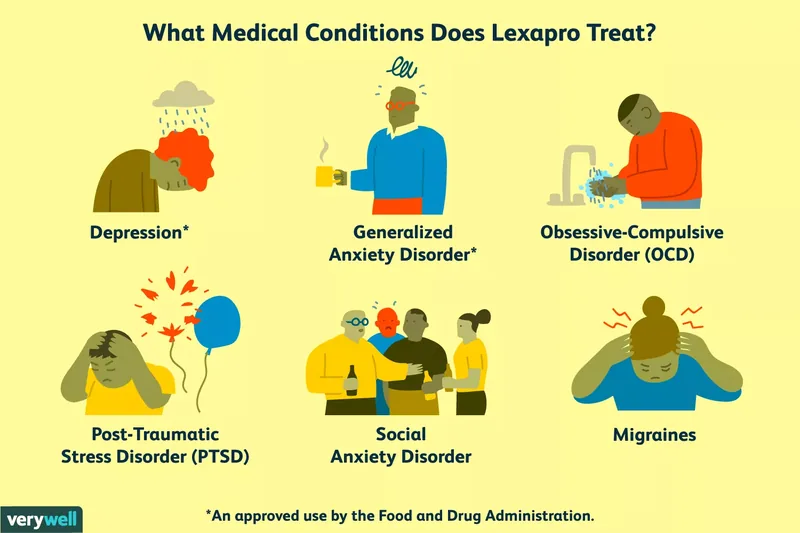
- Ketamine, primarily an anesthetic, is increasingly utilized off-label for mood disorders and chronic pain due to its therapeutic potential.
- Groundbreaking research indicates that low-dose ketamine infusions are a safe and effective option for patients with chronic refractory pain.
- The study highlights significant improvements in pain symptoms, daily functioning, and quality of life for participants.
- Further randomized controlled clinical trials are essential for potential FDA approval and wider adoption.

Source: StockSnap from Pixabay
1. Understanding Ketamine: Beyond Anesthesia
Ketamine, a Schedule III controlled substance, has long been recognized for its potent anesthetic properties, primarily FDA-approved for surgical procedures. However, its unique pharmacological profile, particularly its interaction with NMDA receptors, has spurred growing interest in its therapeutic applications beyond the operating room. For decades, clinicians have observed its capacity to provide significant pain relief, leading to its off-label use as a third- or fourth-line treatment for individuals experiencing chronic pain. This exploratory use underscores a persistent need for innovative solutions in pain management, especially as patients seek alternatives to opioids or when other therapies prove ineffective.
The off-label use of ketamine has been constrained by a lack of standardized protocols and persistent safety concerns. These concerns are often amplified by ketamine's public image as a potentially dangerous recreational drug, overshadowing its legitimate medical applications. Media reports linking ketamine to adverse events, such as the tragic death of actor Matthew Perry or discussions around Elon Musk's reported use, contribute to a complex perception. Such controversies inevitably attenuate the availability of robust, quality data on ketamine's efficacy and safety in controlled medical settings (Harvard, 2024). Despite these challenges, the medical community continues to explore its promise, driven by the profound need for new treatment modalities for debilitating conditions.
The scientific pursuit to fully understand ketamine's mechanisms of action and its broader therapeutic potential remains a priority. While it's known to interact with various neurotransmitter systems, the precise way it alleviates chronic pain is still being elucidated. This ongoing research is crucial for developing safer, more effective protocols and for gaining wider acceptance among both medical professionals and the public. The journey from a surgical anesthetic to a potential chronic pain miracle drug highlights the dynamic nature of medical discovery and the continuous effort to improve patient care.
2. The Groundbreaking Cleveland Clinic Study
A recent study, considered one of the largest of its kind, has provided compelling evidence that low-dose ketamine infusions are both safe and significantly effective for patients struggling with chronic refractory pain. This severe form of pain is notoriously persistent, impacting individuals physically, mentally, and emotionally, often showing little response to conventional medical interventions. The research marks a crucial turning point, offering a rigorously analyzed dataset that reinforces ketamine's therapeutic promise in a controlled clinical setting.
The study meticulously analyzed data from 1,034 chronic pain patients who underwent a five-day outpatient low-dose ketamine infusion protocol. Conducted at the Cleveland Clinic's Center for Comprehensive Pain Recovery between May 2021 and October 2024, the sheer scale of this investigation lends substantial credibility to its findings. This comprehensive approach allowed researchers to gather extensive real-world data on patient responses, treatment completion rates, and adverse events, providing a robust foundation for future clinical practice and policy decisions. The results, published in Regional Anesthesia & Pain Medicine [2], represent a significant stride in validating ketamine's role in pain management.
Participants received subanesthetic doses of ketamine, specifically half a milligram per kilogram of body weight, administered over 40 minutes for five consecutive days. This carefully calibrated protocol aimed to maximize therapeutic benefits while minimizing potential side effects. An impressive 86.1 percent of patients successfully completed the entire five-day treatment regimen, indicating good tolerability and adherence to the protocol. The high completion rate is particularly noteworthy for a treatment targeting chronic pain, where patient dropout can often be a challenge (Harvard, 2024). This structured approach underscores the feasibility of outpatient ketamine treatment, making it more accessible to a broader patient population.
3. Remarkable Patient Outcomes and Sustained Benefits
The impact of the Cleveland Clinic study on patient quality of life was profound, measured using the National Institutes of Health's PROMIS tool, which comprehensively assesses physical, mental, and social health. Patients reported notable improvements across several key domains, demonstrating that ketamine found effective for chronic pain extends beyond mere symptom reduction. Between 20 to 46 percent of participants achieved meaningful improvements in their daily functioning, indicating a tangible return to activities previously limited by pain. This included better management of fatigue, greater satisfaction in social roles, and significantly improved sleep quality, all critical components of overall well-being.
One of the most striking findings was that nearly half of the patients achieved meaningful improvement in pain catastrophizing. Pain catastrophizing, characterized by an exaggerated negative mental set towards pain, is a strong predictor of how well a patient will respond to pain treatment. Reducing this psychological component is vital for long-term recovery and improved coping mechanisms, highlighting how ketamine's effectiveness impacts both physical and psychological dimensions of chronic pain. This suggests that the benefits of ketamine treatment are not just analgesic but also have significant psycho-emotional advantages.
Crucially, the benefits demonstrated by the initial five-day infusion protocol proved to be lasting. Follow-up assessments conducted at three and six months post-treatment revealed sustained improvements across multiple indicators. Patients maintained gains in areas such as depression, social role satisfaction, pain interference, self-efficacy, global health, physical functioning, and pain catastrophizing. This evidence of lasting benefit is a powerful indicator that low-dose ketamine infusions offer more than temporary relief; they provide a foundation for sustained improvement in quality of life. The fact that ketamine found effective in the long term for a significant portion of patients underscores its potential as a transformative therapy, moving beyond acute symptom management to foster prolonged well-being.
4. Addressing Safety and Side Effects
Safety is paramount in any medical intervention, and the Cleveland Clinic study provided reassuring data regarding low-dose ketamine infusions. Despite concerns often associated with ketamine's recreational use, the study observed a remarkably low incidence of adverse events in a controlled clinical setting. Hallucinations, the most commonly reported side effect, were rare and generally mild, not requiring discontinuation of treatment. This contrasts sharply with public perceptions and highlights the importance of distinguishing between supervised medical use and illicit drug use (Harvard, 2024).
Crucially, no serious adverse events were reported across the more than 1,000 participants. Adverse events were rigorously defined as any occurrence necessitating discontinuation of infusions or an emergency medical response, such as abnormal ECG findings, symptomatic hypertension, or hypotension. The absence of such serious incidents in a large cohort undergoing a standardized protocol strongly supports the safety profile of low-dose ketamine when administered by experienced medical professionals. This finding is vital for building confidence in ketamine as a legitimate and safe treatment option for chronic pain patients.
While the study's findings are encouraging, it's important to acknowledge that ketamine is not suitable for everyone. Contraindications for the use of subanesthetic doses of ketamine include pregnancy and a history of ketamine abuse or addiction. These precautions ensure patient safety and responsible medical practice. The careful screening of patients and adherence to strict protocols are essential to mitigate risks and ensure that the benefits of ketamine treatment outweigh any potential harms. This comprehensive approach to patient selection and monitoring reinforces the idea that ketamine found effective within a well-defined and controlled therapeutic framework.
5. Navigating Ketamine's Current Status and Controversies
Despite promising research, ketamine's journey towards widespread acceptance for chronic pain is complex, primarily due to its classification as a Schedule III controlled substance and its current FDA approval limited to general anesthesia [3]. This regulatory status means that its use for chronic pain is considered off-label, a practice where a drug is prescribed for an unapproved indication, dosage, or population. While common in medicine, off-label use often necessitates robust clinical evidence, which studies like the Cleveland Clinic's are now providing to show ketamine found effective in new contexts.
Beyond chronic pain, an increasing number of smaller-scale clinical trials have demonstrated that subanesthetic doses of ketamine can produce significant antidepressant effects in patients with mood disorders, particularly those resistant to standard therapies [4]. This therapeutic promise has unfortunately led to a rapid proliferation of programs and clinicians offering ketamine infusions off-label for psychiatric disorders. While some are reputable, the emergence of clinics with questionable qualifications and experience raises significant concerns about patient safety, ethical practice, and the potential for exploitation of vulnerable individuals seeking relief.
Furthermore, the specter of abuse and addiction remains a significant issue, stemming from reports of cognitive impairment, hallucinations, and bladder dysfunction associated with repeated, high-dose recreational administration of the drug. These concerns, exacerbated by celebrity anecdotes and broader societal perceptions, create a challenging environment for the legitimate medical use of ketamine. Balancing its therapeutic potential with the imperative for patient safety and regulatory oversight is a delicate act. The medical community continues to advocate for rigorous research and standardized guidelines to ensure that this potent compound is used responsibly and effectively, cementing the understanding that ketamine found effective only under strict medical supervision.
6. Future Horizons: The Path to Wider Acceptance
Chronic pain remains a pervasive global health challenge, affecting as many as one in five adults in the United States alone. Many individuals find relief through multidisciplinary care, which includes a diverse array of treatments such as over-the-counter and prescription medications, physical and psychological therapies, alternative interventions, and lifestyle modifications. Yet, for a significant portion, these approaches fall short, underscoring the critical need for novel and more effective treatments. The Cleveland Clinic research provides invaluable data, contributing substantially to the growing body of evidence that low-dose ketamine infusions could become a more widely accepted and vital intervention for this underserved population.
One of the intriguing characteristics of ketamine's pain-relieving quality is that, to this point, its precise mechanism of action remains somewhat unclear. While it's known to interact with NMDA receptors, its broader effects on pain pathways and neuroplasticity are still under active investigation. Unraveling this mystery could unlock even more targeted and effective treatments in the future. The primary advantages highlighted by the recent study for low-dose ketamine include a low tolerance risk, the viability of outpatient administration, and no requirement for general anesthesia. These practical benefits make it an attractive option for patients who might otherwise face more invasive or inconvenient treatment protocols.
For ketamine to achieve potential FDA approval for chronic pain, the next essential steps involve conducting large-scale, randomized controlled clinical trials. These trials are the gold standard for medical research, providing the most robust evidence of a treatment's efficacy and safety compared to a placebo or existing therapies. Such trials will solidify the evidence that ketamine found effective for chronic pain, paving the way for it to move from an off-label option to a recognized, approved treatment. This progression would not only legitimize its use but also facilitate insurance coverage and expand access for the millions who desperately need effective pain relief. The future of chronic pain management looks brighter with ketamine on the horizon, promising a significant shift in how we approach this debilitating condition.
References
[1] Tankha H, Davin S, Lapin B, Li Y, Kennemer A, Schuster A, Xu J, Gopalakrishnan R, Tankha P. Standardized ketamine infusion protocol for chronic refractory pain: a retrospective study of preliminary effectiveness and treatment completion. Reg Anesth Pain Med. 2025 Oct 5:rapm-2025-106907. doi: 10.1136/rapm-2025-106907. https://pubmed.ncbi.nlm.nih.gov/41047247/
[2] https://www.fda.gov/drugs/news-events-human-drugs/understanding-current…
[3] Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB; APA Council of Research Task Force on Novel Biomarkers and Treatments. Ketamine and other NMDA antagonists. Am J Psychiatry. 2015;172(10):950-966.
[4] Wilkinson ST, Toprak M, Turner MS, Levine SP, Katz RB, Sanacora G. A survey of the clinical, off-label use of ketamine as a treatment for psychiatric disorders. Am J Psychiatry. 2017;174(7): 695-696.