Introduction: Understanding Specific Phobias
Living with an intense, irrational fear can be profoundly debilitating, often impacting daily life and personal well-being. This profound distress, far beyond typical fear, characterizes a specific phobia. Many people experience fears or aversions, but it's crucial to differentiate between a common fear and a diagnosable phobia. A specific phobia is an overwhelming and excessive fear triggered by a particular object or situation, invariably leading to avoidance or extreme distress. As of 2025, mental health professionals are finely tuned to the nuances required for accurate assessment.
So, how are specific phobias diagnosed? Specific phobias are diagnosed by qualified mental health professionals, such as psychiatrists, psychologists, or licensed therapists, through a thorough clinical evaluation based on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Text Revision (DSM-5-TR) criteria (Harvard, 2024). This diagnostic process involves assessing the nature, intensity, duration, and functional impairment caused by the fear. For a definitive diagnosis, the fear must be persistent, significantly disruptive to an individual's life, and not better explained by another mental health condition. This detailed approach ensures that individuals receive an accurate understanding of their condition, paving the way for effective treatment.
1. The Definitive Guide to How Specific Phobias Are Diagnosed
The cornerstone of understanding how specific phobias are diagnosed lies in the DSM-5-TR, the authoritative guide for mental health professionals. Since therapists cannot rely on lab tests, they meticulously consult these criteria established by the American Psychiatric Association to ensure an accurate diagnosis. This manual outlines several key indicators that distinguish a specific phobia from a transient fear or aversion, providing a clear framework for assessment. Understanding these criteria is essential for anyone seeking to comprehend their symptoms or support a loved one.
The primary diagnostic criteria for how specific phobias are diagnosed include:
- Unreasonable, Excessive, and Persistent Fear: The individual experiences an immediate, intense, and disproportionate fear or anxiety response when exposed to, or anticipating exposure to, a specific object or situation. This isn't just a fleeting worry; it's a profound and enduring dread. For instance, a fear of flying that causes panic attacks weeks before a trip, even for short flights, points towards this criterion.
- Immediate Anxiety Response: The fear reaction manifests almost instantaneously upon encountering the phobic stimulus. This response is typically out of proportion to the actual danger posed by the object or situation. It's an automatic, often overwhelming, physiological and psychological reaction that individuals struggle to control.
- Avoidance or Extreme Distress: Individuals actively go to great lengths to avoid the feared object or situation. If avoidance is impossible, they endure it with intense anxiety, dread, or significant discomfort. This avoidance behavior can severely limit their life choices and daily activities, impacting social, occupational, and personal spheres.
- Life-Limiting Impact: The phobia must significantly interfere with the individual's normal routine, occupational functioning, academic performance, or social activities and relationships. It's not just an inconvenience; it substantially impairs their quality of life. For example, someone with a severe fear of public speaking might turn down career-advancing opportunities.
- Duration of Symptoms: For both children and adults, the symptoms of the phobia must have persisted for at least six months. This duration criterion helps differentiate between a temporary anxious period and a more ingrained, clinical condition. It ensures that the diagnosis reflects a consistent pattern of distress.
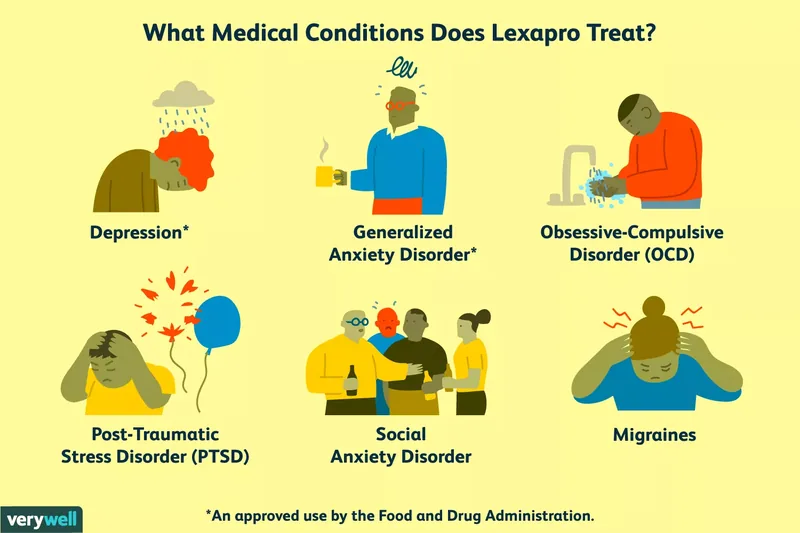
- Not Caused by Another Disorder: Before a specific phobia can be diagnosed, the mental health professional must rule out other anxiety disorders or mental health conditions that might present with similar symptoms. Conditions like agoraphobia, obsessive-compulsive disorder (OCD), social anxiety disorder, or post-traumatic stress disorder (PTSD) need to be carefully considered and excluded as the primary cause of the symptoms.
It's noteworthy that, as per the 2013 DSM-5 update, adults with specific phobias no longer need to recognize the irrationality of their fears to receive a diagnosis. This change acknowledges that insight into the unreasonableness of the fear is not always present, especially during an anxiety attack, making the diagnostic process more inclusive and accurate for how specific phobias are diagnosed in diverse populations.
2. Exploring the Diverse Types of Specific Phobias
Understanding the categorization of specific phobias is crucial for effective diagnosis and treatment planning. The DSM-5-TR identifies five distinct types, each encompassing a range of fears triggered by specific categories of objects or situations. This classification helps mental health professionals pinpoint the exact nature of the phobia, which can influence therapeutic approaches. Recognizing these types also helps individuals understand that their unique fear is part of a recognized pattern, reducing feelings of isolation.
The five recognized types of specific phobias include:
- Natural Environment Type: This category includes fears related to natural phenomena, weather events, and environmental situations. These can be particularly challenging as they often involve elements beyond an individual's control. Examples include astraphobia (fear of thunder and lightning), aquaphobia (fear of water), nyctophobia (fear of darkness), and chionophobia (fear of snow). A new example that has gained more recognition in 2025 is a heightened fear of specific climate-related events, such as extreme heat or wildfires, particularly in areas prone to such occurrences.
- Injury Type (Blood-Injection-Injury Type): This phobia type centers around fears of physical harm, medical procedures, and the sight of blood or injury. Unlike other phobias, this type often uniquely presents with a vasovagal response, leading to a drop in blood pressure and fainting. Common examples include dentophobia (fear of dentists or dental procedures), trypanophobia (fear of injections or needles), and hemophobia (fear of blood). A modern addition might be a fear of certain medical diagnostic tools, such as MRI machines, due to perceived invasiveness or enclosed spaces.
- Animal Type: These phobias are characterized by an intense fear of specific animals or insects. These fears often develop in childhood and can persist into adulthood, significantly impacting daily life if the feared animal is common. Examples include cynophobia (fear of dogs), ophidiophobia (fear of snakes), arachnophobia (fear of spiders), and entomophobia (fear of insects). A burgeoning example in the digital age could be a fear of certain types of rapidly reproducing insects or pests, fueled by viral videos or news reports.
- Situational Type: This category involves fears triggered by specific situations, often those involving confinement or public spaces. These phobias can severely restrict an individual's mobility and independence. Classic examples include claustrophobia (fear of enclosed spaces), aerophobia (fear of flying), and ablutophobia (fear of washing or bathing). A contemporary instance might be a fear of using ride-sharing services, perhaps stemming from a perceived lack of control or safety concerns, which can significantly limit transportation options in urban areas.
- Other Types: This comprehensive category includes any specific phobias that do not fit neatly into the other four classifications. This ensures that all valid specific phobias can be accurately diagnosed and addressed. Examples often include fears of specific objects, sounds, or experiences, such as a fear of dolls (pediophobia), emetophobia (fear of vomiting), or phonophobia (fear of loud sounds). Another unique example could be a fear of certain textures or materials, leading to avoidance of specific clothing or objects, demonstrating the wide spectrum of how specific phobias are diagnosed.
Understanding these distinctions helps in tailoring therapeutic interventions, as some types, like blood-injection-injury phobia, may require slightly different management strategies due to their unique physiological responses.
3. Unraveling the Root Causes of Specific Phobias
The development of specific phobias is a complex interplay of various factors, encompassing an individual's inherent characteristics, genetic predispositions, and life experiences. It's rarely a single cause but rather a convergence of vulnerabilities that culminates in an intense, irrational fear. As researchers continue to explore the neurobiology and psychological underpinnings of anxiety, our understanding of these root causes deepens, informing more targeted prevention and intervention strategies in 2025.
Key factors contributing to the development of specific phobias include:
- Temperament: An individual's innate temperament plays a significant role in their susceptibility to anxiety disorders, including specific phobias. Research consistently suggests that people who exhibit higher levels of behavioral inhibition – a tendency to be shy, withdrawn, and fearful in novel situations or around unfamiliar people – have an elevated risk for developing various anxiety conditions (Fox & Pine, 2012). This temperament can make an individual more sensitive to perceived threats and less resilient to stressful experiences, laying groundwork for how specific phobias are diagnosed later in life.
- Genetics: There is compelling evidence that specific phobias can have a genetic component. Individuals who have a family member with an anxiety disorder or a specific phobia are more likely to develop some form of phobia themselves (Van Houtem et al., 2013). This doesn't mean phobias are directly inherited like eye color, but rather that a genetic predisposition for anxiety or a more reactive stress response can be passed down. This genetic vulnerability interacts with environmental factors, increasing the likelihood of a phobia manifesting.
- Experiences (Learning Experiences): Traumatic or highly stressful experiences are a well-documented catalyst for the formation of specific phobias. This is often referred to as classical conditioning, where a neutral object or situation becomes associated with a terrifying event. For instance, a single incident of being bitten by a dog can lead to the development of cynophobia (fear of dogs). Similarly, witnessing a terrifying car accident could lead to a specific phobia of driving or riding in cars. Even indirect experiences, such as observing someone else's traumatic event or repeatedly hearing frightening stories about a particular object or situation, can contribute to the development of a phobia. This observational learning, or vicarious conditioning, highlights how fears can be "learned" without direct personal trauma. Furthermore, cultural narratives and media portrayals can also shape and reinforce certain fears, contributing to the context in which specific phobias are diagnosed.
Understanding these multifaceted causes helps in developing a holistic approach to treatment, addressing not only the symptoms but also the underlying vulnerabilities and learned associations that maintain the phobia. This comprehensive perspective is vital for long-term recovery and resilience.
4. Effective Treatment Pathways for Specific Phobias in 2025
While specific phobias can be profoundly distressing and significantly impair an individual's quality of life, the good news is that highly effective treatments are available. In 2025, advancements in mental health care continue to refine these pathways, offering hope for reducing or even eliminating symptoms. The primary approaches typically involve a combination of psychotherapy and, in some cases, medication, tailored to the individual's specific needs and the nature of their phobia. The goal is to help individuals regain control over their lives and reduce the impact of their fears.
- Psychotherapy: This remains the gold standard for treating specific phobias, with several techniques proving highly effective. The most commonly used and evidence-based psychotherapies include:
- Exposure Therapy: This technique involves gradually and progressively exposing the individual to their feared object or situation in a safe and controlled environment. The exposure is paired with relaxation strategies to help the individual manage their anxiety. Over time, repeated exposure helps to habituate the fear response, reducing or extinguishing the phobia (Harvard, 2024). For example, someone with arachnophobia might first look at pictures of spiders, then watch videos, then observe a spider in a sealed container, eventually progressing to holding one. This systematic desensitization is incredibly powerful.
- Cognitive-Behavioral Therapy (CBT): CBT is a broad therapeutic approach that helps individuals identify and challenge the automatic negative thoughts and dysfunctional beliefs that contribute to their phobic reactions. By learning to reframe these thoughts and develop more realistic perspectives, individuals can change their emotional and behavioral responses to the feared stimulus. CBT often incorporates elements of exposure therapy, making it a comprehensive treatment for how specific phobias are diagnosed and managed (Kaczkurkin & Foa, 2015). In 2025, virtual reality (VR) exposure therapy is becoming more widespread, offering immersive and controlled environments for exposure without the logistical challenges of real-world scenarios.
- Medication: While medication is typically not used as a standalone treatment for specific phobias, it can be a valuable adjunct, particularly for managing severe physical and emotional reactions. Medications may be prescribed to help alleviate acute anxiety symptoms, allowing individuals to better engage with psychotherapy. Common medications include:
- Beta-blockers: These can help manage the physical symptoms of anxiety, such as a racing heart or trembling, often prescribed for situational use before an exposure.
- Benzodiazepines: These are fast-acting anti-anxiety medications that can provide immediate relief but are generally used for short-term, acute symptom management due to their potential for dependence.
- Antidepressants (SSRIs/SNRIs): While primarily used for depression and generalized anxiety, some antidepressants can help reduce overall anxiety levels, making individuals more receptive to therapy.
It's critical to note that individuals with specific phobias also face an elevated risk for suicide, and these phobias commonly co-occur with other mental health conditions like panic disorder, PTSD, and substance use disorder (American Psychiatric Association, 2022). Therefore, seeking appropriate and timely treatment is not just about managing fear but is essential for overall mental health and safety. If you or someone you know is experiencing suicidal thoughts, please reach out to the National Suicide Prevention Lifeline at 988 for immediate support.
5. Preparing for Your First Consultation: A Proactive Approach
Deciding to seek professional help for a specific phobia is a significant and courageous step towards reclaiming your life. To maximize the effectiveness of your initial appointment and assist your therapist in understanding how specific phobias are diagnosed in your unique case, thoughtful preparation is key. Coming prepared allows for a more efficient and productive session, ensuring that all pertinent information is conveyed clearly. This proactive approach not only helps the clinician but also empowers you in your treatment journey.
Here are three essential lists to compile before your first consultation:
- Symptoms List: Detail all physical and psychological symptoms you experience when confronted with or anticipating your fear. Be specific about your triggers, how you typically cope with your fear (e.g., avoidance, distraction), and any factors that seem to worsen or alleviate your anxiety. For example, if you have a fear of heights, note if dizziness, heart palpitations, or a sense of impending doom occurs. Document how long these symptoms typically last and how they impact your daily activities. This comprehensive list helps the therapist differentiate between a generalized anxiety and how specific phobias are diagnosed based on concrete manifestations.
- Personal Life Overview: Create a list of any significant stressors, changes, or challenges currently present in your life. This includes relationship issues, work-related pressures, academic difficulties, or major life transitions. It's also important to note seemingly positive changes, such as a promotion, a new relationship, or a move to a new city, as even positive events can sometimes induce stress and anxiety. Providing this context helps your therapist understand the broader landscape of your mental well-being and identify potential contributing factors to your phobia.
- Medication and Supplements List: Accurately list all prescription medications, over-the-counter drugs, vitamins, herbal supplements, and even regularly consumed substances like caffeine or herbal teas. Include dosages and how frequently you take them. Some substances can influence your mental state, mimic anxiety symptoms, or interact with potential treatments. For instance, certain stimulants can exacerbate anxiety, while some herbal remedies might have unforeseen effects. This information is critical for your therapist to develop a safe and effective treatment plan.
During your appointment, you'll have a valuable opportunity to ask questions. Don't hesitate to prepare a few in advance to ensure all your concerns are addressed. Consider asking:
- "What treatment options do you recommend for my specific phobia, and what does each involve?"
- "How can I best manage my other health conditions or life stressors while undergoing treatment for my phobia?"
- "If I commit to the recommended treatment plan, what kind of improvement can I realistically expect to see, and over what timeframe?"
Being well-prepared fosters a more collaborative relationship with your therapist and sets a strong foundation for your path to overcoming your specific phobia.
6. Addressing Common Misconceptions and Failures in Self-Diagnosis
While the internet offers a wealth of information, relying solely on self-diagnosis for specific phobias can lead to significant pitfalls and delays in appropriate care. Many common misconceptions exist about what constitutes a true phobia versus a strong dislike or general anxiety. Understanding why professional assessment is critical for how specific phobias are diagnosed is paramount for effective treatment and avoiding potential failures in managing mental health. Self-diagnosis often fails to account for the nuanced criteria laid out in the DSM-5-TR, which requires an expert eye.
One prevalent misconception is that any intense fear automatically qualifies as a phobia. However, a phobia is distinguished by its excessive, irrational, and life-limiting nature, lasting for a significant duration. For example, being nervous about public speaking is common, but avoiding career promotions for years due to crippling fear that causes panic attacks signifies a specific phobia. Without professional guidance, individuals might dismiss their symptoms as mere "shyness" or "nerves," underestimating the severity and impact of a true phobia. This underestimation can lead to chronic avoidance behaviors that further entrench the phobia and narrow an individual's life experiences.
Another failure in self-diagnosis stems from the inability to differentiate specific phobias from other mental health conditions that share similar symptoms. For instance, generalized anxiety disorder (GAD) involves pervasive worry about various aspects of life, while social anxiety disorder focuses on fear of social situations. Agoraphobia, often confused with specific phobias, is a fear of situations where escape might be difficult or help unavailable, typically involving public transportation, open spaces, or crowds. A professional diagnosing specific phobias meticulously rules out these overlapping conditions to ensure the correct diagnosis and, consequently, the most effective treatment plan. Misdiagnosis, whether self-imposed or otherwise, can lead to ineffective interventions, prolonged suffering, and even adverse reactions if treatments for one condition are applied to another.
Furthermore, self-diagnosis often lacks the objective perspective necessary for accurate assessment. An individual's perception of their fear might be skewed by their distress, making it difficult to objectively evaluate the proportionality of their reaction or the true impact on their functioning. A mental health professional, trained in clinical interviewing and diagnostic criteria, can provide this crucial objectivity. They can ask targeted questions, observe behavioral patterns, and utilize standardized assessment tools to arrive at a precise diagnosis. In 2025, with increasing access to telehealth and specialized mental health platforms, seeking professional help has become more convenient than ever, making self-diagnosis less necessary and more avoidable. Trusting trained experts for how specific phobias are diagnosed ensures a more accurate starting point for recovery.
7. Frequently Asked Questions (FAQ) About Specific Phobias
Here are some common questions about specific phobias, answered concisely to provide quick insights.
What is a specific phobia? A specific phobia is an intense, irrational, and overwhelming fear of a particular object or situation that is disproportionate to the actual danger. This fear leads to immediate anxiety and avoidance behaviors, significantly impacting an individual's daily life and overall functioning.
How are specific phobias diagnosed?
Specific phobias are diagnosed by mental health professionals using the DSM-5-TR criteria. This involves a clinical assessment of persistent, excessive fear lasting at least six months, causing significant distress or impairment, and not attributable to another mental disorder.
Can a specific phobia be cured?
While "cured" might be a strong word, specific phobias are highly treatable. With effective psychotherapies like exposure therapy and cognitive-behavioral therapy (CBT), individuals can significantly reduce their symptoms, overcome their fears, and regain full functionality, often eliminating the debilitating impact of the phobia.
What are the most common types of specific phobias?
The five main types are natural environment (e.g., storms), injury (e.g., needles, blood), animal (e.g., spiders, dogs), situational (e.g., flying, enclosed spaces), and other types (e.g., vomiting, loud sounds). These categories help classify the diverse range of specific fears.
Is medication necessary for treating specific phobias? Medication is not usually the primary treatment for specific phobias but can be used as an adjunct to psychotherapy. It may help manage severe anxiety symptoms, such as panic attacks, allowing individuals to better engage with therapeutic techniques like exposure therapy.
How long does it take to treat a specific phobia? The timeline for treatment varies widely depending on the individual, the severity of the phobia, and their commitment to therapy. Some individuals may see significant improvement in a few weeks or months with intensive exposure therapy, while others may require longer-term support.
What should I do if I suspect I have a specific phobia?
If you suspect you have a specific phobia, the best course of action is to consult a mental health professional. They can provide an accurate diagnosis based on DSM-5-TR criteria and recommend an appropriate, evidence-based treatment plan tailored to your specific needs.