When Mark first experienced a surge of energy, he felt unstoppable. Ideas flowed, sleep became optional, and his productivity soared. He launched a new business, invested impulsively, and felt an exhilarating sense of power. Yet, this intense high eventually crashed, leaving him in a profound depression. For Sarah, her heightened periods were different. She felt incredibly creative and social, needing less sleep, and her friends admired her vibrant energy. While these periods were intensely productive and enjoyable, they never spiraled into the same level of chaos or necessitated hospitalization. Both Mark and Sarah live with bipolar disorder, but their experiences highlight a crucial distinction: how mania varies between Bipolar I and Bipolar II. Bipolar I is characterized by full-blown manic episodes, often severe enough to cause significant functional impairment or require hospitalization, while Bipolar II involves less intense hypomanic episodes.
Bipolar disorder is a lifelong mental health condition marked by significant shifts in mood, energy, activity levels, concentration, and the ability to carry out daily tasks. These extreme mood disturbances, known as episodes, impact a person's thoughts, emotions, and behavior. While chronic, the symptoms are manageable with appropriate treatment and support (Harvard, 2024).
Understanding the Bipolar Spectrum
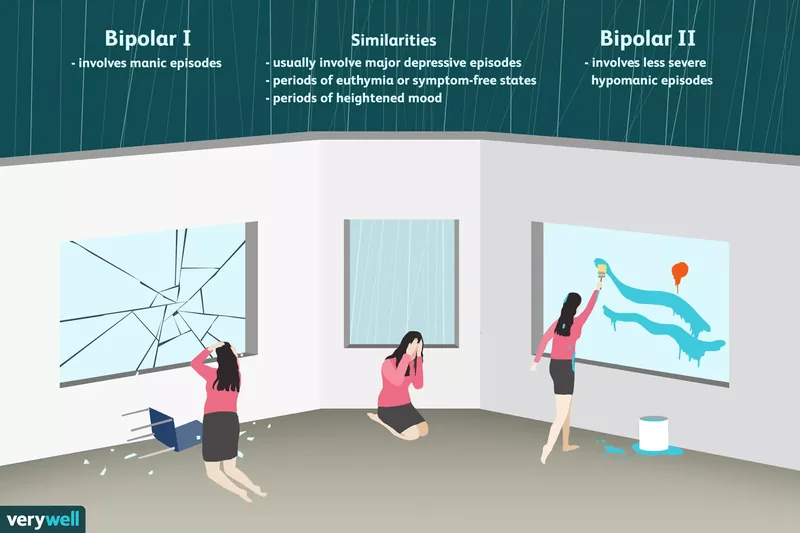
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines two primary types of bipolar disorder: Bipolar I and Bipolar II. The key differentiator, as Mark and Sarah's stories illustrate, lies in the nature and intensity of the elevated mood episodes. Understanding how mania varies between these two conditions is fundamental to accurate diagnosis and effective management.
Depressive Episodes: The Shared Weight
Both Bipolar I and Bipolar II disorders typically involve major depressive episodes. In Bipolar I, a major depressive episode usually occurs but isn't a mandatory diagnostic criterion. However, Bipolar II disorder requires the presence of one or more major depressive episodes for diagnosis. Periods of emotional stability, known as euthymia, can occur in both types (Mayo Clinic, 2023).
Common symptoms experienced during a major depressive episode include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Significant changes in sleep patterns (insomnia or hypersomnia)
- Profound fatigue and loss of energy
- Loss of interest or pleasure in activities once enjoyed
- Unexplained crying spells
- Recurrent thoughts of death or suicide
If you or someone you know is experiencing suicidal thoughts, please seek immediate help. Reach out to a crisis hotline or emergency services.
Mania in Bipolar I: The Surge and the Stakes
A manic episode is a distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least seven days. The severity of these episodes is often profound, leading to marked impairment in social or occupational functioning, or necessitating hospitalization to prevent harm to self or others (APA, 2022).
During a manic episode, individuals may experience:
- A dramatic increase in energy and activity levels
- Intense feelings of euphoria or grandiosity
- Decreased need for sleep, often feeling rested after only a few hours
- Racing thoughts or flight of ideas
- Increased talkativeness or pressured speech
- Distractibility and difficulty focusing
- Engaging in reckless or impulsive behaviors, such as excessive spending, risky sexual encounters, or making significant, ill-advised life changes like impulsively quitting a stable job for a highly speculative venture.
The intensity of Bipolar I mania can sometimes lead to psychotic features like hallucinations or delusions, further complicating an individual's grasp on reality and increasing the risk of dangerous situations.
Hypomania in Bipolar II: The Subtle Ascent
Hypomania, characteristic of Bipolar II disorder, shares many symptoms with mania but is less severe and typically shorter in duration, lasting at least four consecutive days. A crucial distinction is that hypomania does not cause marked impairment in social or occupational functioning, nor does it require hospitalization. Many individuals experiencing hypomania find the increased energy, creativity, and decreased need for sleep enjoyable, often leading to heightened productivity or social engagement (National Institute of Mental Health, 2023).
While hypomania might feel less disruptive than full mania, it's important to recognize its impact. For instance, Sarah, in her hypomanic phases, might take on too many projects, leading to burnout and subsequent depressive crashes, even if her functioning isn't completely impaired during the high. This difference in severity is key to understanding how mania varies between the two types.
Unraveling the Roots: Causes and Diagnosis
The exact cause of bipolar disorder remains complex, but research points to a combination of genetic, biological, and environmental factors. Genetics plays a significant role, as evidenced by studies showing a higher concordance rate in identical twins compared to fraternal twins (Barnett & Smoller, 2009).
Other contributing factors include:
- Brain Circuitry: Abnormalities in brain structure and function, particularly in areas regulating mood, energy, and executive function.
- Neurotransmitters: Imbalances in brain chemicals like dopamine, serotonin, and norepinephrine.
- Environmental Factors: Stressful life events, childhood trauma, or abuse can trigger episodes in genetically predisposed individuals.
Diagnosing bipolar disorder is a nuanced process. A mental health clinician must conduct a thorough evaluation, ruling out other conditions with similar symptoms, such as schizoaffective disorder, schizophrenia, or other psychotic disorders. Unlike many physical illnesses, there's no definitive blood test or imaging scan for bipolar disorder. Diagnosis relies on a comprehensive assessment of symptoms, medical history, and clinical criteria (APA, 2022).
A detailed diagnostic process often involves ruling out other physical contributions to symptoms through tests like a drug screen, brain imaging (CT or MRI), electroencephalogram (EEG), and various blood tests. Open communication with your healthcare team is vital to ensure an accurate diagnosis and tailor an effective treatment plan.
Navigating Treatment and Support
Treatment for bipolar disorder is highly individualized, depending on the specific type, severity, and frequency of episodes. Mood stabilizers form the cornerstone of treatment, often supplemented by other medications:
- Mood Stabilizers: Medications like lithium are crucial for leveling out mood swings.
- Anticonvulsants: These can also stabilize mood and are often used in conjunction with or as alternatives to traditional mood stabilizers.
- Antipsychotics: Used to manage psychotic symptoms during manic or severe depressive episodes, and newer atypical antipsychotics can also have mood-stabilizing properties.
- Antidepressants: Prescribed cautiously, as they can sometimes trigger a manic or hypomanic episode in susceptible individuals (Culpepper, 2014).
In severe cases, electroconvulsive therapy (ECT) may be considered for rapid relief of severe mania or depression that hasn't responded to other treatments (Singh & Kar, 2017).
Why Both Types Deserve Proper Attention
While Bipolar II is sometimes perceived as "milder" because of the less severe hypomanic episodes, this can be a dangerous misconception. The impact of Bipolar II is significant, often characterized by longer and more intense depressive episodes. Research suggests that individuals with Bipolar II may become less likely to return to full functioning between episodes over time (Maina et al., 2007).
Regardless of whether one experiences full mania or hypomania, understanding how mania varies between the types underscores the importance of proper, consistent treatment. Working closely with a dedicated healthcare team is essential for managing symptoms and improving long-term well-being.
Living with Bipolar Disorder: Coping and Beyond
Coping with bipolar disorder extends beyond medication and therapy. Societal stigma, often stemming from a lack of understanding, can add an extra layer of difficulty (Rössler, 2016). Connecting with others who share similar experiences, whether through support groups or online communities, can provide invaluable validation and practical advice.
Effective coping strategies often include:
- Building a Support Network: Engaging with family, friends, and peer support groups.
- Therapy: Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) can provide tools for mood regulation and stress management.
- Lifestyle Adjustments: Maintaining a consistent sleep schedule, regular exercise, and a balanced diet.
- Self-Monitoring: Using a mood tracker app or journal to identify triggers and early warning signs of an episode. For example, Sarah found that tracking her sleep patterns and daily mood swings helped her recognize the onset of hypomania before it became disruptive.
- Advocacy: Learning about your rights and actively fighting stigma can empower individuals living with the condition.
Bipolar Disorder in Children
Bipolar disorder can manifest in children and adolescents, making early recognition and intervention critical. Parents and caregivers should be attentive to a child's functioning, emotional states, and any family history of the disorder. Prompt diagnosis allows for the establishment of a treatment plan tailored to a child's unique needs, significantly improving outcomes (Birmaher, 2013).