It is possible to have high-functioning depression, a term that describes individuals who experience significant depressive symptoms internally while outwardly appearing to manage their daily lives effectively. This hidden struggle often goes unnoticed by others, leading to a profound sense of isolation and a delay in seeking crucial support. While not an official medical diagnosis, understanding the concept of high-functioning depression is vital for recognizing the nuanced ways mental health challenges can manifest. In the first 100 words, it’s clear: yes, you can appear fine to the world even when battling serious internal sadness, fatigue, and hopelessness.
The Nuance of ‘High-Functioning’ Depression: A Growing Challenge
The concept of ‘high-functioning’ depression has gained significant traction in recent years, particularly in discussions around mental health awareness and destigmatization. This colloquial term highlights a critical aspect of mental illness: its often invisible nature. For many, the idea that someone could be battling severe depression while simultaneously excelling in their career, maintaining social connections, or managing a household seems contradictory. Yet, this is the reality for countless individuals. They might be the successful CEO who feels an overwhelming sense of dread each morning, the diligent student achieving top grades while battling persistent fatigue, or the dedicated parent who feels profoundly empty despite outwardly managing family life.
However, despite its utility in illustrating the hidden aspects of depression, some experts caution against the term’s use. It’s crucial to acknowledge that describing depression as ‘high-functioning’ can inadvertently minimize the severity of symptoms and contribute to harmful stigma. It might create an expectation that individuals should be able to function at a high level regardless of their internal suffering, potentially discouraging them from seeking help. The implication that their depression is “less severe” because they can “function” can lead to self-dismissal of symptoms and a reluctance to engage with professional support, fearing their struggles won’t be taken seriously. In a 2025 context, mental health advocates continue to emphasize that all forms of depression, regardless of outward presentation, warrant attention and treatment. The ongoing challenge remains to foster an environment where individuals feel safe to admit their struggles, even when they appear to have it all together.
Recognizing the Hidden Signs: Symptoms of ‘High-Functioning’ Depression
Even when someone appears to manage their daily responsibilities with ease, they can still experience the profound and debilitating symptoms of depression. The key difference in what might be called ‘high-functioning’ depression is the internal battle versus the external facade. These individuals often become adept at masking their distress, leading others to believe everything is fine. However, behind closed doors, or within their own minds, the emotional and physical toll is significant.
Common emotional symptoms include a persistent feeling of sadness or emptiness that lingers for weeks or months, a profound sense of hopelessness or pessimism about the future, and feelings of guilt or worthlessness that are disproportionate to their circumstances. They might also experience heightened irritability or anxiety, a loss of interest or pleasure in activities they once enjoyed, and a tendency to withdraw from social interactions, even with loved ones. Physically, the symptoms can manifest as chronic fatigue and low energy, making every task feel like an immense effort. Changes in sleep patterns, such as insomnia or excessive sleeping, are common, as are shifts in appetite and weight. Some may experience unexplained physical aches, pains, headaches, or digestive issues that resist conventional treatment, all of which are somatic expressions of their underlying distress. A person with possible high-functioning depression might, for example, diligently complete a demanding work project, only to return home utterly drained and emotionally numb, unable to engage with their family. They might meticulously plan a social event, then feel an overwhelming urge to cancel at the last minute, creating excuses to avoid interaction. These individuals often live in constant fear of their internal struggles being exposed, adding another layer of stress to their already burdened minds. The severity of these hidden symptoms can range from mild to severe, even including thoughts of self-harm or suicide, which are often concealed with extraordinary effort.
Understanding the Roots: Causes and Risk Factors
Depression, in all its forms, is a complex mental health condition that rarely stems from a single cause. Instead, it typically arises from an intricate interplay of various biological, psychological, and environmental factors. Understanding these underlying roots is crucial for appreciating why someone might develop possible high-functioning depression despite appearing outwardly resilient.
One significant factor is brain chemistry, involving imbalances in neurotransmitters like serotonin, norepinephrine, and dopamine, which are essential for mood regulation, sleep, appetite, and energy. While not a complete explanation, these chemical fluctuations can significantly impact emotional well-being. Genetics also plays a substantial role; if you have close relatives with depression, your likelihood of developing the condition increases, suggesting a hereditary predisposition. Beyond biology, life events can act as powerful triggers. Stressful or upsetting experiences such as the end of a long-term relationship, job loss, financial difficulties, or the death of a loved one can overwhelm coping mechanisms and precipitate a depressive episode. Similarly, experiencing trauma, whether in childhood or adulthood, can leave lasting psychological scars that contribute to the development of depression, anxiety, or post-traumatic stress disorder (PTSD) (Harvard, 2024). Furthermore, certain medical conditions like heart disease, diabetes, cancer, or chronic pain are frequently co-occurring with depression. The physical and emotional burden of managing these illnesses can significantly increase the risk of developing depressive symptoms. It’s vital to address depression in these cases, as it can worsen outcomes for the primary health condition. Certain medications can also have depression as a side effect, and the misuse of alcohol or recreational drugs can induce or exacerbate depressive states. Finally, specific personality traits, such as perfectionism, low self-esteem, or a tendency towards self-criticism, can make an individual more vulnerable to depression, especially when combined with other risk factors. These traits can also drive the very “high-functioning” facade, as individuals strive for external validation or fear failure.
Beyond the Label: Diagnosing Depressive Disorders
It’s important to reiterate that ‘high-functioning’ depression is not an official clinical diagnosis recognized by the “Diagnostic and Statistical Manual of Mental Disorders” (DSM-5-TR), the standard guide for mental health professionals. Instead, it serves as a descriptive term for how various recognized depressive disorders can manifest in individuals who outwardly maintain a semblance of normalcy. A mental healthcare provider will assess symptoms against established criteria to determine an accurate diagnosis, which is crucial for effective treatment.
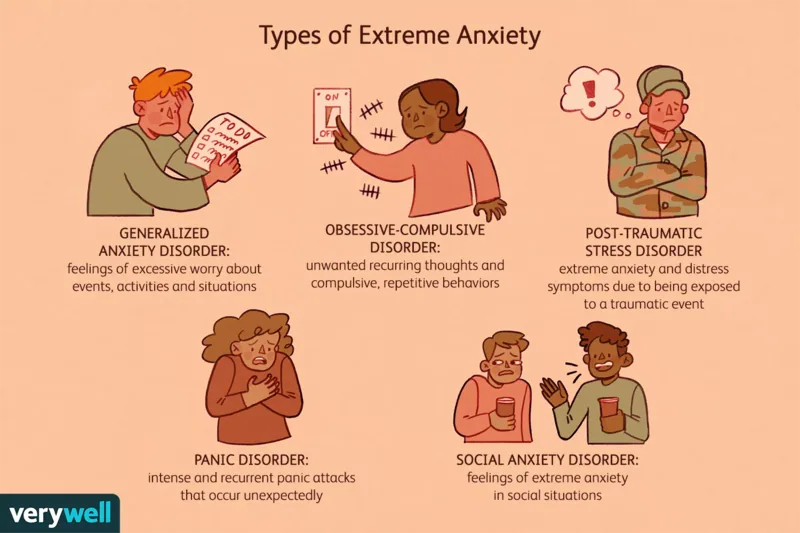
Several types of depressive disorders could align with the layperson’s understanding of ‘high-functioning’ depression:
- Major Depressive Disorder (MDD): Also known as clinical depression, MDD involves a persistent low mood, loss of interest or pleasure, and other significant symptoms lasting for at least two weeks. Someone with MDD might still go to work daily, manage family affairs, and appear productive, all while battling profound internal despair.
- Persistent Depressive Disorder (PDD): Formerly known as dysthymia, PDD involves chronic depressive symptoms that last for at least two years. The symptoms are often less severe than MDD but are enduring, leading to a prolonged sense of sadness, low energy, and lack of motivation. A person with PDD might consistently meet their obligations, but always feel like they’re operating under a cloud.
- Seasonal Affective Disorder (SAD): This form of depression typically occurs during specific seasons, most commonly winter, due to reduced sunlight. Individuals might function well during brighter months but struggle significantly with energy and mood in darker periods, yet still push through daily tasks.
- Perinatal Depression: This encompasses depression during pregnancy (antepartum) and after childbirth (postpartum). New parents, especially mothers, often feel immense pressure to appear joyful and competent, masking severe depressive symptoms.
- Premenstrual Dysphoric Disorder (PMDD): A more severe form of PMS, PMDD involves prominent mood symptoms, including irritability, sadness, and anxiety, in the days leading up to menstruation. Individuals might experience intense emotional swings but manage to navigate work and social commitments.
- Bipolar Depression: Part of bipolar disorder, this involves periods of significant depression alternating with periods of elevated mood (mania or hypomania). During depressive phases, individuals can still maintain aspects of their routine due to the episodic nature of the illness or sheer willpower.
- Psychotic Depression: In severe cases of major depressive disorder, individuals may experience psychotic features like hallucinations or delusions. Even with these extreme symptoms, some may still find ways to conceal their internal reality from others, making the possible high-functioning depression aspect even more complex and dangerous.
A thorough evaluation by a qualified mental health professional is essential to differentiate between these conditions and tailor an appropriate treatment plan. The ability to hide symptoms effectively does not negate their severity or the need for professional help.
The Art of Concealment: Why People Hide Depression
The act of concealing depressive symptoms, particularly in those who are outwardly ‘high-functioning,’ is a deeply ingrained coping mechanism driven by a complex array of psychological, social, and cultural factors. For many, the decision to hide their struggles is not a conscious choice to deceive, but rather a desperate attempt to protect themselves from perceived negative consequences or to maintain a carefully constructed facade.
One common reason stems from family or cultural backgrounds that stigmatize mental illness, teaching individuals to suppress emotions and present a strong, resilient front. In some cultures, admitting to mental health issues can be seen as a sign of weakness or a failure of character, leading to immense pressure to keep silent. Others may subscribe to a belief in self-reliance, thinking they should be able to overcome depression on their own through sheer willpower. This mindset often leads to a pattern of powering through debilitating symptoms, exhausting themselves in the process. The fear of negative impacts on their job and relationships is another powerful motivator. Individuals might worry that disclosing their depression could jeopardize their career advancement, lead to discrimination, or cause loved ones to abandon them. This fear is particularly acute for those in demanding professions or leadership roles, where any perceived vulnerability could be seen as a liability. Furthermore, many people with possible high-functioning depression are simply uncomfortable showing vulnerability or perceived weakness. They may have grown up in environments where emotional expression was discouraged, leading them to internalize the belief that showing distress is unacceptable. This can manifest as perfectionism, where any flaw, including mental health struggles, must be hidden. The pervasive shame associated with having depression is a significant barrier to disclosure. Despite growing awareness, mental illness still carries a stigma, making individuals feel embarrassed or ashamed of their condition. This shame can be compounded by internal comparisons, where they feel they “shouldn’t” be depressed given their apparent success or ideal circumstances. Finally, the profound fear that their life will fall apart and people will abandon them if their depression is discovered creates an immense psychological burden, reinforcing the need for concealment. This fear often leads to a cycle of overcompensation, where they push themselves even harder to maintain appearances, further draining their limited emotional resources.
Paving the Path to Wellness: Effective Treatments for Depression
Despite the outward appearance of managing life effectively, individuals experiencing ‘high-functioning’ depression require and deserve comprehensive treatment. The ability to maintain responsibilities does not diminish the severity of their internal suffering or the necessity of professional intervention. Fortunately, depression is one of the most treatable mental health conditions, with a high likelihood of success when appropriate care is sought (Harvard, 2024). The treatment approach is often multi-faceted, tailored to the individual’s specific needs and the underlying diagnostic criteria.
Therapy is a cornerstone of depression treatment. Cognitive Behavioral Therapy (CBT) is particularly effective, helping individuals identify and challenge negative thought patterns and develop healthier coping mechanisms. Dialectical Behavior Therapy (DBT) can be beneficial for those struggling with intense emotional dysregulation and interpersonal difficulties, offering strategies for mindfulness, distress tolerance, and emotional regulation. Mindfulness-based techniques also play a crucial role, teaching individuals to observe their thoughts and feelings without judgment, which can be invaluable for managing the pervasive sadness and anxiety associated with depression. A skilled therapist can provide a safe, confidential space to explore the reasons behind their need to hide symptoms, working within the context of their work life, family dynamics, and cultural background. This process helps dismantle the shame and fear that often perpetuate the cycle of concealment, empowering individuals to embrace vulnerability and seek genuine support.
For moderate to severe forms of depression, medication often complements therapy. Antidepressants work by helping to balance neurotransmitters in the brain, improving mood, energy levels, and sleep patterns. There are various types of antidepressants, including Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), and atypical antidepressants. Finding the right medication and dosage can be a process of trial and error, requiring patience and close collaboration with a prescribing physician. It’s important to understand that medication is not a “cure-all” but a tool to help alleviate symptoms, making it easier for individuals to engage in therapy and develop lasting coping strategies. Finally, support groups offer an invaluable resource for individuals with possible high-functioning depression. These groups provide a judgment-free environment where individuals can connect with others who share similar experiences. Sharing stories, coping strategies, and mutual encouragement can significantly reduce feelings of isolation and validate their struggles. For those uncomfortable discussing their depression with immediate family or friends, a support group offers a confidential space to build a community of understanding and solidarity.
The Journey Forward: Embracing Support and Long-Term Well-being
The journey through what might be termed ‘high-functioning’ depression is often fraught with internal conflict and the immense pressure to maintain an outward appearance of strength. Yet, it is imperative to remember that depression, regardless of how it manifests, is a legitimate mental health condition, not a character flaw or a sign of personal weakness. The ability to push through daily life while suffering does not make the illness less real or less deserving of compassion and comprehensive care. In fact, many individuals who navigate possible high-functioning depression ultimately choose to become powerful advocates, openly sharing their experiences to destigmatize mental illness and inspire others to seek help. Their resilience, often born from profound struggle, can be a beacon for those still hiding in plain sight.
The prognosis for depression is overwhelmingly positive when treatment is engaged. Modern therapeutic approaches and pharmaceutical interventions have a significantly high likelihood of success, helping individuals not just manage but truly overcome their symptoms. Embracing treatment means acknowledging that you deserve to feel better, that your internal world matters as much as your external accomplishments. It’s an act of self-compassion and courage. For those who find it challenging to accept their diagnosis or who have spent years perfecting the art of concealment, therapy can be particularly transformative. It can provide the tools and support needed to dismantle the psychological barriers that prevent disclosure, fostering a sense of authenticity and genuine connection. Ultimately, the path to long-term well-being involves continuous self-awareness, consistent engagement with support systems, and a commitment to prioritizing mental health. Recognizing that even a ‘high-functioning’ individual can be deeply struggling is the first step towards a life of greater peace, authenticity, and enduring wellness.