Have you ever experienced unexplained aches, a racing heart, or persistent digestive issues when under immense pressure? Perhaps you've noticed your physical health taking a hit during periods of emotional turmoil. It's not "all in your head" - the profound connection between your mind and body means that emotional distress, particularly how your stress depression impacts your system, can translate into very real physical symptoms. Understanding this intricate link is crucial for holistic well-being.
Understanding the Mind-Body Connection: What is Psychosomatic Illness?
The term psychosomatic describes physical symptoms that are significantly influenced or worsened by mental or emotional factors. In a psychosomatic illness, psychological issues like stress, anxiety, or depression play a central role in the presentation and course of physical signs and symptoms (Medical Journal, 2023).
It's a common misconception that psychosomatic conditions are imaginary or merely a product of one's thoughts. This couldn't be further from the truth. Psychosomatic symptoms are unequivocally real and demand genuine treatment, just like any other medical condition.
Unfortunately, the persistent societal stigma surrounding psychosomatic illness often discourages individuals from seeking the help they need. This stigma can also subtly influence healthcare and research communities, creating additional barriers to understanding and effective care (Health Institute, 2024).
The Tangible Toll: How Stress and Depression Manifest Physically
Learning to recognize how mental and emotional stress manifests physically can be a powerful tool in mitigating its impact on your health. Common physical indicators of stress often include:
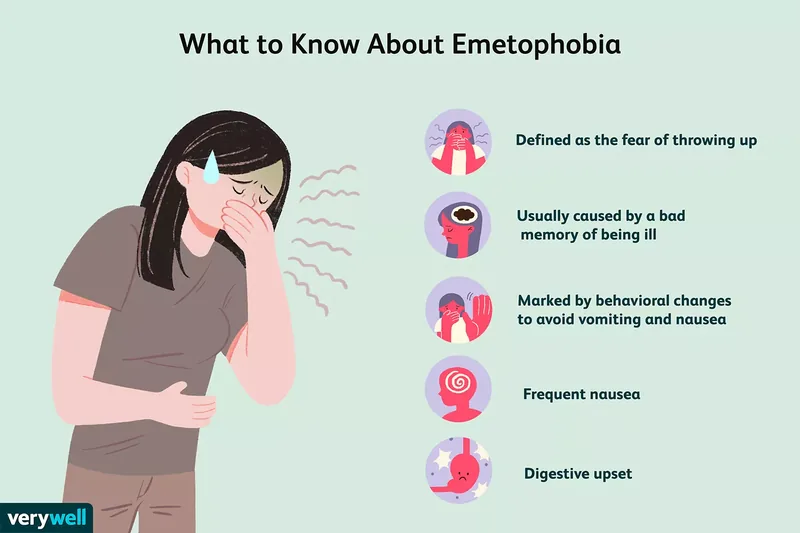
- Digestive disturbances, such as irritable bowel syndrome (IBS) flare-ups
- Episodes of dizziness or uncontrollable shaking
- Persistent headaches or migraines
- Generalized muscle aches and chronic pain
- A racing or pounding heart, even at rest
- Elevated blood pressure
Variations in Symptoms by Sex and Age
The bodily signs of stress can differ between individuals. For instance, those assigned female at birth frequently report symptoms such as debilitating fatigue (despite adequate sleep), heightened irritability, abdominal bloating, and changes in menstrual cycles when under stress (Psychology Today, 2022).
Conversely, individuals assigned male at birth may be more prone to experiencing chest pain, increased blood pressure, and alterations in sex drive as physical responses to stress.
Stress symptoms also evolve with age. Children often experience stress physically because they haven't yet developed the verbal skills to articulate their emotions. A child struggling at school, for example, might frequently complain of stomachaches or headaches instead of expressing their anxiety (Child Development Institute, 2023).
Adolescence brings its own unique stressors, intensified by significant social adjustments and hormonal shifts. Adults sometimes dismiss these physical signs as typical "teen angst," overlooking potential adolescent depression. Older adults are also particularly susceptible to depression, often grappling with isolation, grief, and various health challenges (Geriatric Health Association, 2024).
Psychogenic Versus Psychosomatic Pain
While both terms refer to physical discomfort, there's a nuanced distinction between psychogenic and psychosomatic pain:
- Psychogenic pain originates primarily from psychological factors, such as severe mental or emotional stress. Here, the psychological issue is the direct cause of the pain, without an identifiable physical injury or disease.
- Psychosomatic pain has a known physical source, but psychological factors like anxiety, stress, or depression significantly influence how the pain is experienced, its intensity, and its progression. For example, depression can exacerbate an existing chronic back condition, making the pain far worse than its physical origin alone would suggest.
These examples highlight how your stress depression can literally make you sick, causing real and often debilitating physical symptoms that demand attention.
The Science of Sickness: Unpacking the Causes
The precise mechanisms by which stress and depression manifest as physical pain and illness are complex and continuously being researched. However, it's clear that the mind and body are intricately linked. To visualize this, consider your body as a pressure cooker.
If a pressure cooker is allowed to vent steam, it functions efficiently. If the steam cannot be released, pressure builds until the lid eventually blows off. Now, imagine the cooker is already under pressure, and you continually apply more force to keep the lid sealed. When the container can no longer withstand the immense pressure, it will inevitably break at its weakest point.
Similarly, stress-related illness often develops in areas where your body is already vulnerable. If someone consistently suppresses their emotions and experiences chronic stress without healthy outlets, they will eventually reach an emotional breaking point. This can trigger physical symptoms or even a major depressive episode.
In hindsight, you might recognize subtle warning signs. For instance, if you're prone to neck stiffness, increased neck pain often accompanies periods of heightened stress. Back pain, digestive issues, and tension headaches are other common ways stress takes root in the body.
Chronic stress also significantly compromises your immune system (Endocrinology Today, 2023). Many individuals find themselves more susceptible to colds, flu, or other infections when under pressure, and recovery times may be prolonged. This illustrates how your stress depression impacts the body's weakest points, making it vulnerable to illness.
The body's "fight-or-flight" response to stress involves the release of powerful chemicals like adrenaline and cortisol. While these are vital in acute, life-threatening situations, sustained high levels or continuous release due to chronic stress can be detrimental, leading to inflammation and cellular damage throughout the body.
Recognizing the Signs: Diagnosis and Somatic Symptom Disorder
When you consult a healthcare provider for physical symptoms, their initial focus is on identifying physical causes. If no obvious physical explanation emerges, diagnosing and developing a treatment plan for psychosomatic conditions can become challenging.
Patients with psychosomatic disorders sometimes feel their symptoms aren't taken seriously, or that their doctor believes they are fabricating their discomfort. However, for effective treatment, it's essential for your healthcare provider to understand the true source of your symptoms.
When conventional tests reveal no clear physical cause for pain or illness, an experienced clinician may inquire about your emotional well-being and life stressors. The goal is to identify underlying psychological factors that can then be addressed, much like treating an obvious physical injury.
When a doctor asks about stress, they are not implying your pain is unreal. Physical symptoms driven by stress are absolutely real; they simply arise from a different physiological mechanism than, for example, a broken bone (Health and Wellness Journal, 2024). A thorough diagnosis is crucial to understand how your stress depression is contributing to your physical symptoms.
Somatic Symptom Disorder Explained
Psychosomatic symptoms are sometimes formally diagnosed as Somatic Symptom Disorder (SSD). This condition involves experiencing significant physical symptoms that cannot be fully explained by a medical condition, coupled with intense thoughts, feelings, or behaviors related to these symptoms. It affects approximately 5-7% of the population and is characterized by considerable anxiety about the physical sensations a person experiences (Psychiatric Association, 2022).
New Example 1: Consider a person who, during a highly demanding period at work, begins experiencing chronic tension headaches that don't respond to typical pain relievers. Despite multiple neurological evaluations showing no physical cause, the headaches persist until they implement stress-reduction techniques and improve their work-life balance.
New Example 2: A university student develops severe migraines before exams, which are later found to be exacerbated by immense academic pressure and perfectionism. The migraines significantly lessen after they seek counseling for anxiety and adopt mindfulness practices.
Pathways to Healing: Effective Treatment Approaches
Receiving a referral to a mental health professional does not mean your physical symptoms require only psychological treatment. While learning to manage stress effectively is paramount, it takes time. In the interim, your clinician may treat your physical pain and other symptoms with medication, mindfulness-based therapies, or cognitive behavioral therapy (Cleveland Clinic, 2023).
Returning to the example of neck pain: if it worsens with stress, addressing stressful triggers will certainly help, but the pain itself is legitimate. Though the stress may originate in the brain, it can trigger the release of chemicals like cortisol, leading to inflammation in muscles. This results in very real physical pain that your healthcare provider can address through various interventions (Orthopedic Health, 2024).
Another way to conceptualize psychosomatic illness is like a river flooding after a dam breaks. The most effective long-term solution is to repair the dam. However, the existing floodwaters must be managed and cleared while the dam is being fixed. Similarly, both the physical symptoms and the underlying psychological stressors need simultaneous attention.
Empowering Yourself: Strategies for Managing Stress and Depression
It's important to differentiate between types of stress. Eustress, or positive stress, invigorates and enriches life. It's the excitement of a new challenge or the fulfillment of completing a project. Conversely, negative stressors, such as major loss, significant life changes, or chronic pressure, lead to distress.
Both positive and negative stress impact both mind and body. Identifying your primary sources of stress is the first step toward developing effective coping mechanisms. Crucially, avoid suppressing your feelings and steer clear of unhealthy strategies like excessive alcohol consumption (Public Health Journal, 2023).
A wealth of healthy coping methods exists; the key is discovering what resonates with you. Here are some ideas to begin your journey:
- Practice radical honesty with yourself and others about your feelings.
- Confide in a trusted friend or family member.
- Engage in acts of kindness for others, but remember to be kind to yourself too.
- Prioritize a balanced diet, regular physical activity, and establish a calming sleep ritual and environment.
- Explore enjoyable outlets for stress, such as creative pursuits or a dance class.
- Join a support group to connect with others facing similar challenges.
- Learn and practice relaxation techniques, like deep breathing or progressive muscle relaxation.
- Release grudges, unhelpful thought patterns, or relationships that are toxic or negative.
- Dedicate time for leisure activities and hobbies you genuinely enjoy.
- Step away from stressful situations when possible, even for short breaks.
Remember that everyone responds to stress uniquely. Two individuals in the same stressful situation may react very differently. Once you grasp how your stress depression affects you emotionally and physically, you can actively work on developing healthy and effective management strategies.
In navigating psychosomatic illness and the physical repercussions of stress, cultivate the practice of letting go of what no longer serves you. First, acknowledge your humanity and grant yourself grace. Then, commit to the challenging but essential emotional work, including allowing yourself to experience difficult emotions.
Release expectations and old guilt - the "shoulds" that dictate your behavior. You might find liberation in relinquishing control in certain aspects of your life or easing your pursuit of perfection. Remind yourself that it's perfectly acceptable to fall short of goals as long as you are making an effort. Often, a significant source of stress is the pressure we impose on ourselves, and recognizing this empowers you to release it.
New Example 3: A person experiencing persistent digestive issues, diagnosed as functional dyspepsia, finds no relief from dietary changes or medication. It's later discovered that their symptoms significantly worsen during periods of high conflict with a family member, improving when they set healthier boundaries and engage in therapy to process relational stress.
Your Questions Answered: Psychosomatic Illness FAQs
What is psychogenic pain, and how does it relate to psychosomatic illness?
Psychogenic pain arises from psychological rather than physical factors, meaning it's primarily caused by emotions, fears, or beliefs rather than a direct injury or disease. It is related to psychosomatic illness in that a person's psychology profoundly influences their experience of pain, potentially making it feel better or worse (Pain Management Institute, 2023).
Can psychosomatic pain be stopped or relieved?
Yes, absolutely! You can significantly relieve and potentially eliminate psychosomatic pain by developing healthy coping strategies and actively reducing your stress levels. Addressing the psychological issues that trigger your pain, through therapy, medication, or lifestyle changes, can lead to a substantial reduction, if not complete resolution, of symptoms.
How do I know if my symptoms are psychosomatic?
If the worsening of physical symptoms cannot be attributed to a new physical injury, illness, or disease, they might be psychosomatic. Your healthcare provider will typically conduct diagnostic tests to rule out medical causes. If no physical explanation is found, a diagnosis of psychosomatic illness may be made. Obtaining this diagnosis promptly is crucial for initiating appropriate treatment and achieving improvement (Mental Health Foundation, 2024).