Neuroscience · Mindfulness & Mental Health
The Complete Guide to Ultrasound Brain Therapy
Can sound waves really change your brain without a single incision? Focused ultrasound brain therapy is moving from sci-fi to standard care, offering a non-invasive way to treat tremors, Parkinson’s symptoms, and potentially some psychiatric conditions—without opening the skull.
In under a minute: Ultrasound can be precisely focused through the skull to heat or modulate specific brain regions, helping reduce tremors and movement symptoms and opening new paths for mental health treatment. MRI guidance makes it targeted; decades of neurology research make it credible.
Why This Matters Now
Living with relentless tremors, muscle rigidity, or intrusive obsessive thoughts is more than a medical problem. It erodes identity, independence, and daily confidence. Many people feel trapped between powerful medications with side effects and invasive brain surgery that feels terrifyingly high-stakes.
For millions worldwide, the real challenge is clear: effective brain treatment without losing control over your body, personality, or future options.
Focused ultrasound brain therapies are emerging as a third path—precise, image-guided, and incision-free.
From Submarines to the Ultrasound Brain Revolution
The journey of ultrasound brain technology begins far from the clinic.
Early in the 20th century, scientists developed ultrasound to detect submarines using reflected high-frequency sound waves. This sonar work revealed two key properties still central today:
- Reflection: Waves bounce off solid structures, allowing imaging.
- Energy deposition: At certain intensities, ultrasound generates heat and biological effects.
These discoveries led first to medical imaging—heart scans, fetal ultrasounds, and organ checks—and later to therapeutic uses. By the mid-20th century, researchers showed focused high-intensity ultrasound could selectively destroy small areas of tissue, including deep brain targets, without cutting through the skin.
Today, guided by MRI and backed by more rigorous safety standards (Harvard, 2024), those early explorations have evolved into clinically approved tools for movement disorders, with expanding research into psychiatric care.
Why Traditional Treatments Aren’t Enough
Before ultrasound emerged as a serious brain therapy candidate, patients mainly faced two options.
1. Medication Limits
For conditions like Parkinson’s disease:
- Levodopa and related drugs can significantly reduce symptoms.
- Over time, many people develop motor fluctuations, involuntary movements, or reduced effectiveness.
- Doses often escalate, bringing nausea, low blood pressure, sleep issues, or mood changes.
For psychiatric disorders (OCD, depression, anxiety):
- Many patients cycle through multiple medications and therapies.
- A meaningful subset remains treatment-resistant, experiencing ongoing distress despite best-practice care.
2. Invasive Brain Surgery Challenges
Deep Brain Stimulation (DBS) transformed care for many patients. But it comes with:
- Surgical implantation of electrodes and a chest battery
- Infection and bleeding risks
- Device maintenance, battery changes, and programming demands
- Psychological barriers: "Brain surgery" feels irreversible and frightening
Problem: People who are suffering, yet hesitant or unsuited for invasive procedures, are left in a dangerous gap—under-treated, demoralized, and often isolated.
This is the space where focused ultrasound brain therapy is beginning to matter.
How Ultrasound Affects the Brain: The Science
Ultrasound brain approaches use high-frequency sound waves delivered through the skull and shaped into precise focal points.
Key Mechanisms
Thermal Ablation (High-Intensity Focused Ultrasound)
Concentrated ultrasound energy heats tissue at a tiny focal spot, destroying it while sparing surrounding areas.Neuromodulation (Low-Intensity Focused Ultrasound)
Lower intensities can modulate brain activity without destroying tissue, influencing how neurons fire. This area is rapidly evolving, with early work from Stanford researchers and others exploring mood, pain, and cognitive effects.Blood-Brain Barrier Opening Paired with microbubbles, ultrasound can temporarily open the blood-brain barrier to help medications reach specific brain regions more effectively—an emerging approach in neuro-oncology and neurodegeneration.
In simple terms: high-intensity ultrasound can create permanent, targeted changes, while low-intensity ultrasound offers reversible tuning of brain circuits.
Safety in 2025
Modern systems integrate:
- Real-time MRI guidance
- Continuous temperature monitoring
- Strict dose limits based on decades of physics and biology data
This allows a level of precision and control that early experiments lacked, aligning with current safety expectations (Harvard, 2024).
Focused Ultrasound for Parkinson’s and Tremor
Featured Answer (snippet-ready):
Focused ultrasound for Parkinson’s disease and essential tremor uses MRI-guided high-intensity beams to heat and ablate tiny brain regions involved in abnormal signaling. The procedure is incision-free, performed in a single session, and can rapidly reduce tremor or rigidity in carefully selected patients.
Current Clinical Uses
MRI-guided Focused Ultrasound (FUS), including platforms such as Exablate Neuro, is now used in many centers for:
- Essential tremor that does not respond to medication
- Tremor-dominant Parkinson’s disease
- Select cases with other Parkinsonian motor symptoms
How It Works (Step-by-Step Framework)
- Assessment: Neurologist evaluates symptom pattern, imaging, overall health, and previous treatments.
- Targeting: MRI identifies the precise brain nucleus causing abnormal signaling.
- Test sonications: Low-energy pulses confirm correct target by producing temporary, reversible effects.
- Thermal lesioning: Energy is increased until a permanent micro-lesion is created.
- Immediate feedback: Tremor or rigidity often improves during the procedure.
Real-World Examples
- A programmer with severe essential tremor returns to accurate typing the week after treatment.
- A retired teacher with medication-resistant Parkinson’s tremor regains the ability to hold a cup and sign documents.
- A chef, previously unable to plate dishes steadily, resumes part-time work after symptom relief.
These outcomes are not universal, but they illustrate why ultrasound brain therapy is seen as a proven option—not just an experiment—for selected movement disorders.
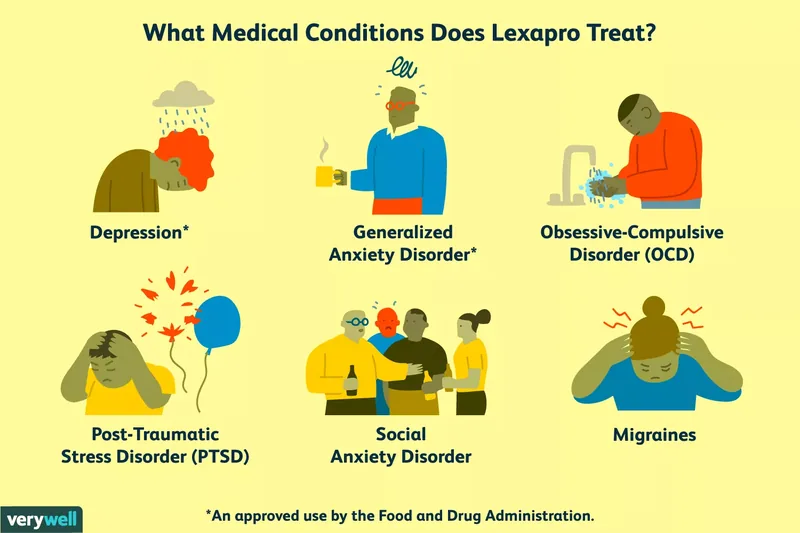
Can Ultrasound Help Mental Health?
Featured Answer (snippet-ready): Emerging research suggests focused and low-intensity ultrasound could safely target brain circuits linked to OCD, depression, and addiction. Early trials show promise, but psychiatric uses remain limited, carefully regulated, and should be viewed as experimental rather than mainstream in 2025.
The Promise
Psychiatric disorders involve dysregulated brain circuits, not character flaws. That makes them, in principle, candidates for:
- Circuit-level modulation (changing activity without removing tissue)
- Ultra-precise lesions in rare, severe, treatment-resistant cases
South Korea’s approval of focused ultrasound for certain OCD cases reflects this shift toward biologically-grounded interventions.
Why It’s Still Emerging
- Brain networks for mood, anxiety, and compulsions are complex and overlapping.
- Overly aggressive interventions risk personality changes or cognitive side effects.
- Ethical concerns about consent, identity, and long-term impact demand caution.
Stanford researchers and other teams are running controlled trials on low-intensity focused ultrasound neuromodulation for depression and OCD. The direction is hopeful, but for now, standard therapies (CBT, medication, lifestyle interventions) remain foundational, with ultrasound reserved for research or very specific severe cases.
Key insight: Non-invasive does not mean casual. Psychiatric ultrasound interventions must be guided by robust science, ethics, and long-term follow-up.
Implementation Timeline: What Patients Can Expect
If you or someone you love is exploring focused ultrasound for tremor or Parkinson’s, a realistic path looks like this.
1. Evaluation (Weeks 0–4)
- Neurology referral and confirmation of diagnosis
- Review of medication history and response
- Cognitive and mental health screening
- MRI to ensure suitable brain anatomy
2. Decision & Preparation (Weeks 4–8)
- Discuss benefits, risks, and alternatives (DBS, meds, no procedure)
- Review insurance or funding options
- Hydration, medication adjustments, and pre-procedure imaging as advised
3. Procedure Day
- Head shaved at target area for accurate ultrasound transmission
- Patient lies in MRI scanner with a specialized ultrasound helmet
- Awake, able to give real-time feedback
- Several hours total, home typically the same day
4. First 1–4 Weeks Post-Procedure
- Tremor or symptom change often visible immediately
- Mild headache, temporary imbalance, or numbness possible
- Follow-up visits to track stability and side effects
5. 3–12 Months and Beyond
- Many maintain substantial benefit
- Some may experience partial symptom recurrence
- Ongoing neurology care remains essential—this is a treatment, not a cure
For psychiatric applications, expect a much more conservative trajectory: research screening, trial protocols, and close monitoring rather than immediate widespread clinical use.
Troubleshooting & FAQs
What are the main risks of focused ultrasound brain therapy?
- Localized numbness or tingling
- Balance issues or gait disturbance
- Rare, more serious complications if heat affects nearby tissue
Most side effects are minimized through stepwise energy increases and MRI monitoring.
Who is a good candidate?
You may be considered if:
- You have disabling tremor or Parkinson’s symptoms despite optimal medication.
- You are medically high-risk for open surgery or strongly prefer a non-invasive option.
- Imaging shows clear targets and no contraindications.
Is ultrasound brain treatment reversible?
- High-intensity thermal lesions are permanent.
- Low-intensity neuromodulation is typically reversible, but still under investigation.
Understanding which approach is being proposed is crucial.
How does this compare with DBS?
- Focused Ultrasound: One-time, incision-free; no hardware; limited adjustability after lesion.
- DBS: Invasive; adjustable and reversible; more data for bilateral and complex symptoms.
Many centers now discuss both options in a shared decision-making model.
Will ultrasound cure Parkinson’s or OCD?
No. Current evidence supports symptom relief, not disease reversal. Lifestyle changes, medication, therapy, sleep, movement, and social support remain essential pillars.
Key Takeaway: Ultrasound brain therapies represent a proven, non-invasive option for select movement disorders and a promising frontier for mental health, grounded in decades of physics, neurology, and imaging research. As standards tighten and evidence grows, this technology is reshaping how we think about changing the brain—safely, precisely, and with more respect for the person living inside it.